Enhancing Cardiac Rehab Participation
Introduction
Cardiac Rehabilitation program is referred to the supervised medical program which is designed for improving the cardiovascular health of individuals who have experienced heart attack, heart surgery or angioplasty (Anderson et al. 2016). The program includes exercise and counselling of patients to ensure their healthy living. However, in many cases, several clinical and psychological barriers act to avoid individuals with heart diseases include in the rehabilitation programs that negatively affect their life. Thus, in this study, the barriers encountered by the patients are to be identified and addressed by developing strategies so that improved participation rate for the cardiac rehabilitation programs can be achieved ensuring healthy life to the individuals.
Research Rationale
There are different strategies exists to improve participation rates in cardiac rehabilitation program yet increased rate of participation gaps are seen. In the study by Sumner et al. (2016), it is informed that from 2012 to 2015 out of 234,736 patients referred to attain cardiac rehabilitation program in England, there were 141,648 participants who enrolled in the program, 97,406 initiated to participate in the program and out of the participants who initiated only 37.2% of them completed the whole program. The figures indicate that though enrolment in the cardiac rehabilitation program is high but only few individuals are actually participating and completing the program to ensure their good health. In another study by de Vries et al. (2015), which was executed in Netherlands it was reported that out of 35,919 patients with acute coronary syndrome or coronary revascularisation who are referred to cardiac rehabilitation program from 2007-2010 only 11,014 patients (30.7%) were seen to register in the program and from them 80% completed the program. Thus, it indicates that major number of individuals with cardiac issues avoided participation in the CR program raising the issue of risk of further heart diseases among them. The gaps of participation in cardiac rehabilitation (CR) program has become an issue because it has resulted patients to remain vulnerable to experience relapse of their heart diseases as their behaviour and actions required for controlling their condition could not be achieved. It is evident as the study by Sunamura et al. (2017) informs that lack of completion of CR programs leads individuals with heart issues experience diabetes, increase smoking, face anxiety, experience great attack and others. The CR programs informs the patients who have already suffered heart disease about the way to reduce negative activities like smoking and drinking, educated about exercises to avoid further relapse of acute myocardial infarction or other heart issues, control anxiety, stress; inform regarding the way to take their medication and control their diet and others (Chou et al. 2016). Thus, the lack of participation has led individuals with heart issues remain vulnerable even after effective medical intervention and treatment.
Dig deeper into Education's Dual Role in Development with our selection of articles.

The gaps in participation in cardiac rehabilitation (CR) program have currently become an issue because an increased number of patients with heart diseases have shown relapse of their problem. It is evident from the study by Cleland et al. (2019) where it is informed that 40% of the patients showed relapse of their heart issues after withdrawal from the treatment and another 10% have their medicines and treatment to be reinstated as a result of uncontrolled hypertension. Thus, this study is going to highlight the key barriers experienced by patients that are making them avoid successful participation in cardiac rehabilitation programs to avoid further relapse and effective control of their health condition.
Background of the Study
The cardiac rehabilitation (CR) program provides detailed information to the patients and their family members through support and advice regarding the way patients who have suffered heart diseases are to return to their normal life. In different researches, it is shown that cardiac rehabs are able to reduce risk of heart attack for individuals, lower their chances of readmission to hospitals and creates a positive effect on the well-being of the individuals (Pack et al. 2015). The individuals or patients who attend the CR programs are found to have less anxiety, control over stress and depression which are associated to create risk of heart attack (Andraos et al. 2015). The cardiac rehabilitation programs usually last 10-12 weeks and each session runs for 2 hours approximately during which different physical exercises are taught, psychological support, information regarding diets to be maintained, education regarding the significance of avoiding drugs and alcohol along with smoking for healthy heart and other are provided (bhf.org.uk, 2019). In some cases, it is seen that people feel nervous to initiate and participate in the cardiac rehabilitation programs as they fear of not being able to execute the information as provided like others. This nature of confusion acts to create barriers to participation in the CR programs as people feel they cannot effectively use the services for their purpose and thus spending time in this aspect is useless (Park et al. 2017). In the UK, US and Canada it is seen that prescribing patients with cardiac disease are not standard form of practice performed by the physicians due to which 70-80% of patients who are eligible to participate in the program are not enrolled in the cardiac rehab after discharge from the hospital (Grace et al. 2011). Thus, it indicates that lack of effective referral from the physicians is creating barriers for participation in the CR programs. The lower socio-economic status of the individuals poses barriers to participation in the CR programs. This is because poor individuals do not have effective financial ability to spend money for availing cardiac rehabilitation programs after spending much of their finances to avail treatment for heart diseases (Ruano-Ravina et al. 2016). The presence of co-morbidities such as osteoporosis, diabetes, urinary incontinence and others poses barriers to participate in the CR programs. This is because individual with such condition does not have the physical ability to execute exercises suggested in the programs for remaining healthy making them ignore to enrol for the programs (Aragam et al. 2015).
The family responsibilities are also found to create barriers to participation in CR programs apart from different other factors as mentioned in different studies (Salavati et al. 2016). There has been no single study where it has been found that all the barriers related to the CR programs are identified as one. Thus, to understand in detail the way various barriers to participation in CR program affects to create gap of enrolment in the process detailed systematic review of different articles has to be made in framing this study.
Aim of the Review
The focus on the review is to identify the barriers experienced during participation in cardiac rehabilitation programs by patients.
Search Strategy
The Systematic Review is the process in which the already present findings of healthcare studies which are carefully designed is summarised that helps to deliver an increased level of evidence on the significance of clinical intervention. The reviews to be executed are complicated in nature and they mainly depend on the available clinical trials (Moher et al. 2015). The benefit of using systematic review is that they allow the reliable collection of data as the evidence gathered are from scientific studies that are effectively developed under the proper supervision of the clinical researchers. In addition, it allows cumulative evidence to be added that are developed over time on the study topic (Shamseer et al. 2015). Thus, to minimise biases and to develop evidence through transparent approach the systematic review is to be used as the search strategy.
Database
The electronically moderated database and search engines are to be used for collecting evidence regarding the study because searching online for information assists the researcher to gather wide variety of updated evidence which is relevant to the study topic. This nature of searches eases the process of collecting data in comparison to physically searching for information within the pages of each book from the library (Bannay et al. 2016). The databases that are used for executing this study include CINAHL, PubMed, Google Scholar, MEDLINE, etc. The following databases are selected as they are key areas where wide variety of diverse healthcare resources regarding different clinical topic are stored. Thus, using them would help the researcher to gather and compile wide number of information regarding the study topic.
Search Terms
The specific use of properly framed search terms assists the researcher to find out relevant articles and journals that are related to the topic, in turn, helping to execute a comprehensive study. The search terms to be used for executing this study are: "Cardiac rehabilitation program", "barriers to enrol CR programs", “cardiac arrest patients” and others. During the search, the terms are to be properly customised based on the nature of search engine and database to be used. In addition, the terms are used for executing manual search to gather information from physically available books and journals.
Research Question Formulation
In order to formulate the specific research question, the PICO tool is to be used. The PICO tool is referred to as a pattern that is used in performing evidence-based study for framing and answering a healthcare-related query. It is the frequent tool used for developing literature searches in systematic reviews (Eriksen and Frandsen, 2018). As commented by Miglus and Froman (2016), the research question is needed to be relevant and directly related to the research problem and they are to be phrased in such a way so that it ensures the search conducted develop proper answer for raised problem in the study. Therefore, to develop a relevant question the PICO tool is to be used for the research. The PICO framework stands for population, Intervention, Control and Outcome (Eriksen and Frandsen, 2018). The problem is the key issue that has led to develop the execution of the study which in this research is barriers experienced that hindered the participation of patients and individuals in cardiac rehabilitation (CR) programs. The intervention is the action that is taken to resolve the raised issue which in this study is strategies for resolving barriers to participation in cardiac rehabilitation programs. In this study, no control or comparison group is present. The outcome is the final result to be received which in this study would be improved participation in the cardiac rehabilitation programs by patients and individuals.
The research question formulated is: What are the barriers to participation in cardiac rehabilitation programs and the way to resolve it?

Inclusion and Exclusion criteria
The factors and/or characteristics that are required to be present in the study topic is known as inclusion criteria whereas the exclusion criteria are the characteristics need to be excluded from the study to ensure this smooth execution is known as exclusion criteria (Demaerschalk et al. 2016). In the study, the non-English, non-academic, not fully accessible journals and articles are the exclusion criteria along with articles that do not include information about barriers to participate in cardiac rehabilitation programs is to be excluded. The academic and English Journals that are fully accessible and contain information regarding barriers to CR programs participation are to be included. The English and academic journals that are fully accessible are included as English is the only known language by the researcher and the fully accessible article provided relevant and detailed information to the gathered for the study. The studies which are conducted from 2009-2018 are to be included and studies before 2009 are to be excluded as it would lead to collect most current information regarding the topic.
Take a deeper dive into Addressing Cardiovascular Diseases with our additional resources.

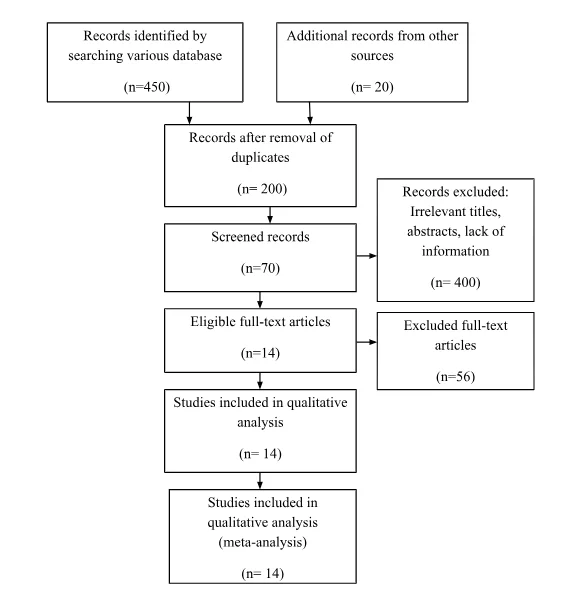
PRISMA Chart
Review and Discussion
Theme 1: Barriers to participate in cardiac rehabilitation program
In overall Europe, the percentage of people who are admitted to cardiac rehabilitation (CR) program is estimated to be 30% while the figures in the USA indicate 20-30% (Abreu et al. 2018). The reason behind such gaps is found to be presence of diverse barriers experienced among patients that hindered their participation in cardiac rehabilitation program. One of the barriers experienced is improper referral by healthcare providers and physicians of the patients suffering from heart diseases. This is evident as most of the physicians are seen to lack familiarity or detailed information regarding CR programs as well as its relevant location which makes them less inclined to effectively refer a patient for the program (Soroush et al. 2018). In contrast, the study by Gravely-Witte et al. (2010) informs that standards referral system used by the physicians to refer patients have shown lower rates of participation by the patients compared to the ones who are referred through automatic referral and liaisons. This is because standard referral is made by the physicians at their discretion where they decide whether or not to refer a patient to CR program whereas automatic referral system is being supported by clinical policies and guidance making the process compulsory to be implemented by the physicians.
The lack of education is another barrier that acts to reduce registration rates for cardiac rehabilitation (CR) programs. The poor patients without effective education regarding CR programs are unable to understand its benefits for survival making them ignore to participate in the programs, in turn, reducing enrolment rate for the programs (Ragupathi et al. 2017). Thus, the feeling of the patients that the CR programs are not necessary for their improved health creates barrier in CR program participation. In comparison, the study by Resurrección et al. (2018) informs that the patients avoid enrolling to execute actions mentioned in the CR programs to be safe because of distance issues from their home to rehabilitation centres. The distance issues create barriers for those patients who are unable to drive or do not have effective socio-economic condition to bear the increased cost of transportation required to reach the recommended rehabilitation centres for the specific patients. The obligation of the patients to return to work after treatment creates barriers to participate in cardiac rehabilitation programs. This is because such obligation provides less time and scope for the patients to learn and attend the actions mentioned in the programs for their benefit as including in such program would need them to spend the time used for work. Moreover, failure to attend work makes the patients lose their job and become economically unstable and to avoid such consequences they avoid joining the program (Moghei et al. 2017). In contrast, the study by Supervía et al. (2017), highlights the psychosocial barriers faced by patients to participate in CR programs such as social deprivation, lower socioeconomic status, depression, lack of motivation and others. The social deprivation of the patients who require CR programs creates barrier in participation because individuals who have lower social status are discriminated and not provided proper information regarding CR programs making them unable to enrol (Buys et al. 2016). Thus, ignorance and discrimination towards participation as a result of being socially deprived creates barriers for patients to enrol in CR programs. The presence of depression and anxiety creates barriers to participate in CR programs because the patients who are depressed with their health condition feels that the CR programs could not benefit them to survive. In addition, these patients lack the concentration to understand and execute the actions and exercises mentioned in the programs making them avoid continuing in the program (Zullo et al. 2017). In contrast, the study by Supervía et al. (2017) informs that family responsibilities, work pressure, exercising as tiring and comorbidities create barriers to participate in cardiac rehabilitation programs. This is because family responsibilities provide less time for the patients to attend the programs properly and continue them as it would mean they are ignoring the needs of the family. Moreover, considering exercise as tiring makes individuals avoid participation in CR programs so as to avoid them unnecessary pain. In comparison, the study by Hamilton et al. (2018), informs that lack of awareness regarding CR programs acts as barriers for its participation. This is because without proper awareness the individuals lack understanding regarding the need and benefit of the programs, where they are delivered, how to be registered and who is going to deliver them, in turn, making them fails to include and enrol in the program.

Theme 2: Strategies to overcome barriers experienced to participate in cardiac rehabilitation program
The reduction in drive time of patients to the cardiac rehabilitation centre for accessing the program is able to improve participation for the programs. This is evident from the study by Suskin et al. (2019) where it is informed that more patients enrolled in CR programs when their drive time was less than 60 minutes. Thus, the physicians require considering the geographic location of the patients while referring them to CR programs so that the individuals can be referred to closet centre to their location. The use of modern technologies is to be made for delivering and expanding awareness regarding cardiac rehabilitation program. This is because it would help to expand knowledge and information regarding the program through effective supervision to target individuals without hindrance or geographic barrier (Ades et al. 2017). In the study by Salavati et al. (2016), it is recommended that home-based cardiac rehabilitation programs are to be used alternative to hospital-based programs. This is because it would help the individual avoid hindrance to travel as well as experience familiar environment to execute suggested actions. The physicians while referring patients to the CR programs required to properly resolve their fear of feeling of pain due to exercise so that they can be motivated to enrol in the program (Ades et al. 2017). Moreover, the patients suffering from depression regarding their heart issues and lost hope to live are to be informed about the benefits of the CR programs. This is going to motivate them to participate in the CR programs (Dalal et al. 2015).
Conclusion
The systematic review of different articles and journals regarding barriers to participation in cardiac rehabilitation programs informs that different clinical and psychosocial factors are mainly responsible for the condition. The studies reveal that psychosocial barriers include social deprivation, lower socio-economic condition, lack of motivation, ineffective transportation cost, geographic issues and others. The clinical barriers include presence of comorbidities, depression and feat of pain from exercise, referral issues and others. In order to resolve them, effective strategies such as reduction in drive time, home-based cardiac rehabilitation programs, motivation to accept CR programs through proper delivery of knowledge and others are to be implemented.
Future Research
The study can be used as a reference in future to understand the way different barriers to participation in the cardiac rehabilitation programs are raised and faced. In future, the research can be further explored to compare its findings with the real-life data gathered to ensure whether or not the findings are true. Moreover, the study in future can be used for comparative analysis and be used as reference in developing effective strategies to overcome barriers to participation in the CR programs.
References
Abreu, A., Mendes, M., Dores, H., Silveira, C., Fontes, P., Teixeira, M., Santa Clara, H. and Morais, J., 2018. Mandatory criteria for cardiac rehabilitation programs: 2018 guidelines from the Portuguese Society of Cardiology. Revista Portuguesa de Cardiologia (English Edition), 37(5), pp.363-373.
Ades, P.A., Keteyian, S.J., Wright, J.S., Hamm, L.F., Lui, K., Newlin, K., Shepard, D.S. and Thomas, R.J., 2017, February. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. In Mayo Clinic Proceedings, 92(2), pp. 234-242.
Anderson, L., Oldridge, N., Thompson, D.R., Zwisler, A.D., Rees, K., Martin, N. and Taylor, R.S., 2016. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. Journal of the American College of Cardiology, 67(1), pp.1-12.
Andraos, C., Arthur, H.M., Oh, P., Chessex, C., Brister, S. and Grace, S.L., 2015. Women’s preferences for cardiac rehabilitation program model: a randomized controlled trial. European journal of preventive cardiology, 22(12), pp.1513-1522.
Aragam, K.G., Dai, D., Neely, M.L., Bhatt, D.L., Roe, M.T., Rumsfeld, J.S. and Gurm, H.S., 2015. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. Journal of the American College of Cardiology, 65(19), pp.2079-2088.
Bannay, A., Chaignot, C., Blotière, P.O., Basson, M., Weill, A., Ricordeau, P. and Alla, F., 2016. The best use of the Charlson Comorbidity Index with electronic health care database to predict mortality. Medical care, 54(2), pp.188-194.
Buys, R., Claes, J., Walsh, D., Cornelis, N., Moran, K., Budts, W., Woods, C. and Cornelissen, V.A., 2016. Cardiac patients show high interest in technology enabled cardiovascular rehabilitation. BMC medical informatics and decision making, 16(1), p.95.
Chou, A.Y., Prakash, R., Rajala, J., Birnie, T., Isserow, S., Taylor, C.M., Ignaszewski, A., Chan, S., Starovoytov, A. and Saw, J., 2016. The first dedicated cardiac rehabilitation program for patients with spontaneous coronary artery dissection: description and initial results. Canadian Journal of Cardiology, 32(4), pp.554-560.
Cleland, J.G., van Veldhuisen, D.J. and Ponikowski, P., 2019. The year in cardiology 2018: heart failure. European heart journal, 40(8), pp.651-661.
Demaerschalk, B.M., Kleindorfer, D.O., Adeoye, O.M., Demchuk, A.M., Fugate, J.E., Grotta, J.C., Khalessi, A.A., Levy, E.I., Palesch, Y.Y., Prabhakaran, S. and Saposnik, G., 2016. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 47(2), pp.581-641.
Gravely-Witte, S., Leung, Y.W., Nariani, R., Tamim, H., Oh, P., Chan, V.M. and Grace, S.L., 2010. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nature reviews cardiology, 7(2), p.87.
Moghei, M., Turk-Adawi, K., Isaranuwatchai, W., Sarrafzadegan, N., Oh, P., Chessex, C. and Grace, S.L., 2017. Cardiac rehabilitation costs. International journal of cardiology, 244, pp.322-328.
Pack, Q.R., Squires, R.W., Lopez-Jimenez, F., Lichtman, S.W., Rodriguez-Escudero, J.P., Lindenauer, P.K. and Thomas, R.J., 2015. Participation rates, process monitoring, and quality improvement among United States Cardiac Rehabilitation Programs: a national survey. Journal of cardiopulmonary rehabilitation and prevention, 35(3), p.173.
Resurrección, D.M., Motrico, E., Rubio-Valera, M., Mora-Pardo, J.A. and Moreno-Peral, P., 2018. Reasons for dropout from cardiac rehabilitation programs in women: A qualitative study. PloS one, 13(7), p.e0200636.
Salavati, M., Falahinia, G., Vardanjani, A.E., Rafiei, H., Moosavi, S. and Torkamani, M., 2016. Comparison between effects of home based cardiac rehabilitation programs versus usual care on the patients’ health related quality of life after coronary artery bypass graft. Global journal of health science, 8(4), p.196.
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P. and Stewart, L.A., 2015. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj, 349, p.g7647.
Soroush, A., Heydarpour, B., Komasi, S., Saeidi, M. and Ezzati, P., 2018. Barriers for the referral to outpatient cardiac rehabilitation: A predictive model including actual and perceived risk factors and perceived control. Annals of cardiac anaesthesia, 21(3), p.249.
Supervía, M., Medina-Inojosa, J.R., Yeung, C., Lopez-Jimenez, F., Squires, R.W., Pérez-Terzic, C.M., Brewer, L.C., Leth, S.E. and Thomas, R.J., 2017. Cardiac rehabilitation for women: a systematic review of barriers and solutions. In Mayo Clinic Proceedings, 92(4), pp. 565-577.
Suskin, N.G., Shariff, S.Z., Garg, A.X., Reid, J., Unsworth, K., Prior, P.L. and Alter, D., 2019. Importance of Completing Hybrid Cardiac Rehabilitation for Long-Term Outcomes: A Real-World Evaluation. Journal of clinical medicine, 8(3), p.290.
Zullo, M.D., Gathright, E.C., Dolansky, M.A., Josephson, R.A., Cheruvu, V.K. and Hughes, J.W., 2017. The Influence of Depression on Utilization of Cardiac Rehabilitation Post-Myocardial Infarction: A Study of 158,991 Medicare Beneficiaries. Journal of cardiopulmonary rehabilitation and prevention, 37(1), p.22.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



