A Critical Analysis of Service Improvement
Introduction
The service improvement in healthcare is the process of combining efforts of all staffs and employees to develop changes which would lead to improved patient outcomes, professional development, care approaches and care system performance. In this report, the service improvement required for the NHS is to be critically analysed for improving patient safety along with tools and models to be used for supporting the improvement is to be critically discussed. In addition, the leadership qualities are to be evaluated in making the change. For those seeking comprehensive guidance, healthcare dissertation help can provide valuable insights. In the report, a reflection of my role of student nurse transition to registered nurse is to be explained where the roles and responsibilities to be played are to be acknowledged.

Importance of change in NHS
The change is required within the NHS so that the care services and support can be improved to meet the ever-changing needs of the population (kingsfund.org.uk, 2016). This is because it would help the service providers deliver care that meets the needs and demands of patients, in turn, offering them care satisfaction as well as ensure good health. In the medical field, huge advancement in research, as well as medical technology, is seen that has lead immense changes in the way care services and treatment is to be provided along with patients are to be diagnosed for their health issues (England.nhs.uk 2014). Therefore, change in the NHS is required so that they can adapt their care services and way of diagnosing patients with the advanced technology and research to deliver better care within less time and effort to service users.
The National Early Warning Score (NEWS2) score informs the degree of illness within patient and cues when critical care intervention is to be taken for which patient (rcplondon.ac.uk, 2017). Therefore, NEWS2 score is important to take immediate and proactive care for patients to avoid worsened health condition. Thus, the proposed change to be implemented is the establishment of a system that informs staffs to know when the NEWS2 score for the patients is to be rechecked so that the health professionals do not miss the opportunity to detect deteriorating health of a patient.
Looking for further insights on Service Improvement? Click here.
Listening to Patients
The active listening to patients is important by the nurses and healthcare staffs as it conveys respect and dignity towards the individuals helping to build trust and allows health professionals understand the needs of the patients according to which the care is to be developed (Selby et al. 2017). Thus, listening to the patients in the NHS is to be promoted as it would result the nurses and health professional arrange satisfactory care services for the patients as well as develop trusted relationship between one another allowing the staffs to deliver care without accusation or avoidance from the service users. The Francis Report which is developed based on analysing the failures of Mid Staffordshire Hospital informs that there was lack of systematic procedure to listen to the complaints regarding service failure from the patients which led to worsened the condition in the hospital (nmc.org.uk, 2015). This informs that listening to the patient is important as it would lead the staffs to understand where services are not properly managed that they are to improved to ensure delivering quality care and promote better health of the individuals.
The Francis Report informs that the failure in care in the hospital occurred as there is a culture among the staffs who were avoided listening to the service users and were discouraged to report regarding failures and concerns related to care services (Halligan, 2013). It informs that listening to the patients is important to encourage whistleblowing by the staffs. This is because listening makes nurses or staffs get aware regarding the extent to which the patients are suffering making them develop compassion and responsibility to take active steps in reporting the problem so that better health condition of the patients can be promoted. The barrier in listening to patients is that the staffs may not understand the information provided by patients with learning disability, have dementia and others as they lack proper ability to verbally communicate their needs (Moore et al. 2017).
The Friends and Family Test (FFT) is framed by the NHS to receive feedback from the patients for determining their level of satisfaction regarding care services and how likely they are going to refer it to their friends and family members (NHS.uk, 2018). This allowed active listening to the patients as the feedback received included the positive and negative factors of the services based on which the care is to be further improved. However, the test was performed online and created barriers for the patients to participate who lack knowledge regarding the way to use technology to report their grievances and feedback (nhs.uk, 2018). The HealthWatch England is developed under the Health and Social Care Act 2012 which is statutory body with the purpose to speak up regarding changes in car services to be required on behalf of patients by analysing their needs, experiences and concerns regarding care (healthwatch.co.uk, 2019). The advantage of using this body as receiving feedback from the patient is that it allowed individuals who are unable to report their views due to fear of repercussions, inability to access certain feedback methods, having learning disability and other to report their perception regarding services.
Rationale for improving services at the NHS
The NHS access patient’s feedback through postal survey organised across different areas. The information gathered is analysed consistently and systematically and the response to the demanded change based on the analysed feedback is executed by the NHS through improvement and alterations in care services (nhssurveys.org, 2018). However, the delivery of altered and improved care services by the NHS is found not to reach the target and needy service users within time and in appropriate manner. This is evident as nearly 1/5th of the individuals identified by the NHS to be in desperate need for hip replacement are found to be suffering from pain due to lack of timely services (dailymail.co.uk, 2019). In addition, the overall waiting time for patients in England is found to reach all-time high where 4.4 million patients are waiting more than normal time to receive healthcare procedure. Among them, ½ a million have already been waiting for more than four months to receive healthcare procedure for their health condition (dailymail.co.uk, 2019). Therefore, the quality of response to meet the needs of the service users by the NHS within time is found to be poor even though active steps are promised being taken.
The feedback provided by the patients to the NHS reports that they are facing lower quality care from health professionals. The NHS by analysing the feedback found that the quality of care is deteriorating as there is lack of proper amount of healthcare staffs and in response, they tried recruiting more staffs (nhssurveys.org, 2018). However, it is seen that there is lack of nearly 75,000 doctors as well as nurses within Britain only compared to other developed countries and there is lack of effective qualities and skills to provide care among many of the existing staffs (telegraph.co.uk, 2015). Thus, it indicates that quality of response by the NHS to change regarding care services is poor as they are unable to make proper strategic changes through recruitment of trained staffs and management of quality health professional as well as healthcare staffs to deliver better care to the service e users. Therefore, it has led NHS to provide poor, hindered and untimely care to many patients deteriorating the healthcare scenario in the country.
The NHS to currently improve their healthcare service quality is required to perform healthcare audits and chart audit. The healthcare audits are referred to the process in which current practices are compared with the desired standard by the health professionals and organisation to determine the changes in care is to be made for delivering improved quality healthcare support to the service users (Brookes and Baker, 2017; Hut-Mossel et al. 2017). The information of the healthcare audits is to be used by the NHS to make active changes in the care delivery process to meet the care support with the determined standards of care set by the government. The chart audit is referred to the process in which the skills and performance of the healthcare professionals are determined for identification of area and skills to be improved to make them deliver better and efficient services (Barick et al. 2018). This chart audit is to be used by NHS to examine the skills of the existing professionals and based on the reports are to arranged training and development programs for the staffs to improve their skills and knowledge for providing better quality car which is not yet established.
The benchmarking is the process in which performance of the organisation is determined against the best approaches which are considered in the industry (Purushotham et al. 2018). Thus, the improvement in care quality within the NHS is to be made through internal and external benchmarking process where NHS would determine which are their best practice that is to be implemented in delivering high-quality and improved care. The success of the improvement for the NHS is to be measured by continuous monitoring and evaluation of the performance of the healthcare professionals and staffs. This is because continuous monitoring and evaluation assist to determine the way the changed service is being implemented at each step and whether or not they are being properly followed to deliver care (Sharma et al. 2017). In addition, statistical methods along with survey and patients outcomes are to be used for measuring the improvement of NHS.
The interprofessional collaboration enhance the safety of service users as in the process diverse professionals with expertise in different healthcare fields are involved who through partnership, cooperation and sharing knowledge determines the best outcome for the patients. This, in turn, allows prevention of unnecessary healthcare errors and promote safe patient outcome as the right care approach in the proper way is implemented (Foronda et al. 2016). For instance, the National Patient Safety Agency (NPSA) is developed where interprofessional through collaboration at work monitor and ensures safe patient care including analysis of reports of prescription and medication error. In addition, they also look over the safety of the patients by evaluating the cleanliness, food and design of hospital (gov.uk, 2011). The National Institute of Health and Care Excellence (NICE) is national body where through interprofessional collaboration they offer guidance regarding the way healthcare is to be improved to ensure safe care support to the service users (nice.org.uk, 2019).
Models and tools for supporting improvement of service
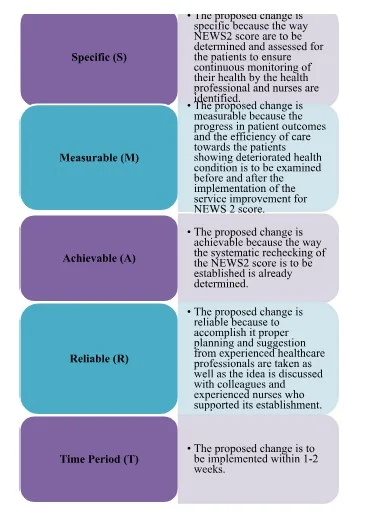
The SMART goals, SWOT analysis and circles of influence are the tools used for supporting service improvement. The SMART goals assist to develop clarified ideas, focus efforts, and make use of effective time and resources in productive manner as well as increase the change to achieve the proposed change. The SMART goals stand for specific, measurable, achievable, relevant and time period (Chaballout et al. 2017). The benefit of using SMART goals is that it provides clarified framework regarding the way the change in service is to be achieved. In addition, the tool assists in effective planning, motivating and determining results to be received through service improvement and allows staying on track while making changes (Chaballout et al. 2017). However, the SMART goals provide limitation in failing to set proper objectives to make successful service improvement (Oueida et al. 2019).
The SWOT analysis tool allows determining strength, weakness, opportunity and threat regarding changes to be made (Moro Visconti, 2016). The benefit of using SWOT analysis is that it allows effective strategic planning and assist in building change based on the strengths to reverse weakness as well as overcome threats through maximisation of opportunity (Chen et al. 2015). The limitation of SWOT analysis is that its too much structure leads to poor decision-making in turn leading to fail in accomplishing improvement (Moro Visconti, 2016). The circles of influence refer to the concerns which can be controlled to manage service improvement. The benefit of circles of influence is that it allows individuals to easily separate factors they can control and does not control in making service improvement (Mosadeghrad, 2015). However, the limitation is that it does not inform the way the concerns that cannot be controlled can be influenced in supporting effective change or service improvement (Khayal and Farid, 2018).
The SMART Tool is to be used for setting proper objectives that would support fulfilling the proposed service improvement. This is because it allows individuals making change to stay on track as well as develop clarified goals and make effective planning to accomplish change in easier and less complicated manner.
The change model used for making service improvement in healthcare includes Kotter's 8 stage model, Lewin's Three Stage change model and the PDSA cycle. The strength of using Kotter’s 8-step model is that it provides a robust checklist of elements which are required during the successful change process. However, the limitation of the model is that it is mechanical and weak in providing proper guidance in sustaining a change (Kuo and Chen, 2019). The Lewin's change management model is that it provides simple system to be followed in making the change. However, the limitation is that it does not provide scope to determine how much time the change is to be finally established and sustained (Ellis and Abbott, 2018). The strength of using PDSA cycle in making change is that it allows improving confidence, offering flexibility, assisting in determining side-effects of decisions and minimising resistance in making a sustained change or improvement (Christoff, 2018). However, the limitation of PDSA cycle use in making proposed change is that wrong conclusion may be drawn that may lead to develop failed action in making the change (Reed and Card, 2016).
The proposed change of implementing system for rechecking of NEWS2 score for patients to ensure their proper care for controlling deterioration of their health is to be done by following the PDSA cycle. This is because the PDSA cycle is the change management which allows effective planning as well as determining the side-effects of change to develop a successful alteration which would sustain the change (Mazzocato et al. 2016). The Kotter’s model is not used as it does not ensure sustained chain management and Lewin’s model is not used because it cannot inform within how much time the change can be established in turn leading to raise confusion in sustainability of the change (Kuo and Chen, 2019).). The PDSA cycle stands for Plan, Do, Study and Act steps. In the planning stage, the way change to be made along with time, the reason behind it and who are to be involved in the change determined (Mazzocato et al. 2016). The proposed change is establishing a system which informs staffs when the NEWS2 score for the patients is to be rechecked. In order to accomplish the service improvement, a NEWS2 scoreboard is to be established outside each ward and bed of the patient and the stakeholders to be involved are physicians, nurses and ward manager of the hospital.
The nurses caring for the patients have the role to check NEWS2 score for each individual on regular basis and mention them on the scoreboard along with the time and date when they were taken. The nurses on each shift are to follow the board to determine when the next rechecking of NEWS2 score for the patient is to be made. The physicians visiting the patients are to examine the scoreboard to determine which patient's health is deteriorating and required immediate change in care to improve their health. The ward manager has the role to check whether the scoreboard is regularly updated in proper manner to ensure the NEWS2 score of the patients is checked at proper interval to easily determine their health condition. Moreover, the physicians, nurses and ward manager are to work collaboratively in ensuring proper NEWS2 score is determined on regular basis with each other’s assistance. In the Do phase, the planned change is implemented in the organisation (Leis and Shojania, 2017). In this phase, the roles and responsibilities mentioned for each professional are to be performed in collaborative manner.
In the Study phase, the implemented change is to be measured and its impact is to be reflected (Parker et al. 2018). Thus, in this phase, the ward manager and nurses along with physicians are to assess whether by installation of the rechecking the NEWS2 scoreboard for the patients have offer help in improving patient outcome in the ward. This is to be done by analysing the health progress of each patient and accessing feedback from the patients and their family members. This is because positive health progress of patients along with positive feedback and improved satisfaction of care would indicate that the installation of the service improvement was able to bring better healthcare opportunity for the individuals in the ward. The Act stage informs the next change cycle to be planned based on the implementation of the proposed change (Coury et al. 2017). Thus, in this stage, further aspects to be improved in the proposed change to maintain its sustainability is to be determined and implemented
Critical Analysis of change management
The supporting and sustaining the mentioned proposed change or service improvement in the NHS would be done by creating awareness among the internal stakeholders regarding its importance and essential impact on the health of the service users as well as the organisations. As mentioned by Wright and Endsley (2017), building awareness regarding the significance of a change among the stakeholders helps in sustaining the change. This is because it makes the stakeholders to be involved in the change have clear vision regarding the desires and intentions to be achieved through the change or improvement which in turn empowers them to determine the way to act in collaborative manner to ensure change is made in the best possible way. Thus, creating awareness among the nurses, physicians and ward manager that rechecking of NEWS2 score daily and in continuous time interval would help in controlling deteriorating health of the patients and better management of the health of critically-ill patients in the ward. In addition, it would make them collaboratively contribute in establishing the change in sustained manner so that effective health outcomes for the patients are achieved continuously.
The proposed change would be sustained in the study by making the stakeholders involved in the process remain motivated and inspired to follow the rules. As mentioned by Hardcastle and Hagger (2016), effective motivation for the stakeholders to follow proposed change makes them develop positive intention to show better efforts in sustaining it. This is because motivation makes the stakeholders understand the value and increased need of establishing the change, in turn, making them offer more productive efforts in implementing it. Thus, the nurses are to be appreciated and shown positive results of improvement of health as well as care support for the patient due to the change to motivate them to offer greater efforts in productive way to sustain the change. As argued by Murphy et al. (2015), lack of motivation to the stakeholders towards making the proposed changed leads them to lose value and lack understanding the change may not be essential as they are not pushed to achieve it. This, in turn, leads towards failure in making the change in sustainable manner as out of motivation and value the stakeholders avoid implementing the change.
The proposed change for the NHS is to be sustained by making the stakeholders have the opportunity to show their involvement and share ideas to progress its further sustainability. As asserted by Willis et al. (2016), creating opportunities for the stakeholders who are making the change to share and implement their ideas in the change contributes towards its sustainability. This is because the stakeholders feel their opinions are valued and they have effective contribution towards launching the extension of the change. As argued by Deeny and Steventon (2015), lack of proper skills and knowledge in making the proposed change among the stakeholders act as barrier which leads the service improvement to lack sustainability. This is because the stakeholders are unable to understand the way they are to act and resources are to be managed to make the change sustain. Thus, the stakeholders in the proposed change that are nurses, ward manager and physicians are to be ensured that each of them has proper skills and knowledge regarding the way NEWS2 score is to be assessed and managed in controlling healthcare for the patients. In case they lack sills, effective training and development program regarding the management of NES2 score is to be provided with each of them.
The lack of receiving feedback from the patients regarding service improvement acts as barrier towards its establishment and sustainability. As commented by Johnson and May (2015), feedback regarding service improvement makes stakeholders involved in the change determine to what extent they have progressed and what further is to be done to more intricately and successfully implement the change. Thus, the patients and their family members are to be provided feedback regarding their satisfaction and concerns about the service improvement made for NEWS2 score. This is because it would make the stakeholders which are the interprofessional understand the extent of achievement they have received through the change and the change to be made in the services further in making the change sustainable to help them deliver better healthcare to the patients. As criticised by Mahanta et al. (2016), lack of effective communication act as barrier which hinders sustaining the change. This is because without communication between stakeholders they are unable to know which parts are played properly and whereas assistance is to be provided in making the proposed change sustain in the healthcare environment. Therefore, the nurses, ward manager and physicians are required to be in continuous communication with another regarding the way they can collaboratively work and assist each other so that rechecking system of NEWS2 score is properly maintained on the scoreboards for assessing the health of the patients.
In order to make the proposed change, the qualities of transformational leader are to be used. As asserted by Thomson III et al. (2016), transformational leaders have the quality to control ego and make informed decision. This is required for making the proposed service improvement as during planning as leader by controlling ego the stakeholders who are involved in the change can be provided opportunity to share their ideas which can be included in making the change. It is going to lead the stakeholders feel valued in turn making them personally engaged and supportive to make the change as well as would make the leader have better information in making better decision regarding the change. As commented by McCaffrey and Reinoso (2017), transformational leaders develop tough decisions as they execute it through clarified vision and goals which are communicated among all in the organisation. Thus, this quality is to be used in making the proposed change as it would make the stakeholders have proper vision of the goal to be achieved in turn making them desired to implement the change.

Transition towards professional practice
The reflection in nursing is important as it allows the nurses to review their activities and practices as well as improve their professional skills and personal knowledge based on the review to ensure their ability to deliver effective quality care to patients (Lestander et al. 2016). The reflective model mentioned by Driscoll is to be used in reflecting the transition to professional practice and my leadership qualities and skills. The Driscoll's reflection model includes three steps which are What?, So What? and Now What? (Stonehouse, 2019).
What?
During the implementation of the proposed change, it was seen that I was clam and constrained the entire time. I interacted with my colleagues to understand their opinion and ideas of establishing NEWS2 scorecard for each patient which is to be updated each day at proper interval of time as well as to be reviewed by the nurses on each shift change to determine whether or not they have to recheck the score to determine health condition of the patient. Moreover, I tried to offer proper reason behind the change I have proposed and how it would improve service quality in the end when established. However, I experienced fear of facing the risks and barriers which may be raised towards hindering the sustainability of the change. In addition, I was at times unable to inspire my colleagues who faced hindrance to cope with the change.
So What?
I feel that I have the quality of transformation leader. This is because the quality of a transformation leader is to keep their ego under control share ideas, ensure collaboration from others in making an informed decision and lead with vision (McCaffrey and Reinoso, 2017). I avoided to show ego as well as by mention the way and reason of service improvement among the colleagues I think I was able to develop proper vision for them to follow the change as seen in case of transformation leader. The transformational leaders also have the quality to take tough decision, face risks and provided proper inspiration to its subordinates (Reichenpfader et al. 2015). However, I felt that I lacked these qualities as I was unable to inspire my colleagues when they were facing issues with implementing the proposed change as well as experienced fear by thinking of the risk which may be encounter that may jeopardise the change.
Now What?
The experiences faced during the proposed change that I have to improve by self-management abilities along with require to develop skills and knowledge regarding the way challenges are to be resolved with confidence during any change to become a proper transformation leader. In future, during the transition from student nurse to registered nurse, I would engage is listening to the patients intricately to understand how service improvements are to be made effectively. Moreover, I would implement lifelong learning to improve my knowledge regarding the way risk to be encountered in service improvement are to be managed to ensure smooth change establishment.
References
- Barick, U., Vijaykanth, A., Bharucha, H., Gowda, A., Patil, A., Bosbach, S. and Zomorodi, B., 2018. Are Retrospective Patient Chart Audits an Affordable and Reliable Answer to Healthcare Data Needs? Assessing the Ground Reality. Biomedical Journal, 1, p.6.
- Brookes, G. and Baker, P., 2017. What does patient feedback reveal about the NHS? A mixed methods study of comments posted to the NHS Choices online service. BMJ open, 7(4), p.e013821.
- Chaballout, B.H., Shaw, R.J. and Reuter-Rice, K., 2017. The SMART healthcare solution. Advances in Precision Medicine, 2(1). pp.66-78.
- Chen, N., Liu, X., Meng, L.I., Guo, S. and Dong, S., 2015. The SWOT analysis on private hospitals in the background of new healthcare reform. Chinese Journal of Health Policy, (8), pp.39-43.
- Christoff, P., 2018. Running PDSA cycles. Current problems in pediatric and adolescent health care, 48(8), pp.198-201.
- Coury, J., Schneider, J.L., Rivelli, J.S., Petrik, A.F., Seibel, E., D’Agostini, B., Taplin, S.H., Green, B.B. and Coronado, G.D., 2017. Applying the Plan-Do-Study-Act (PDSA) approach to a large pragmatic study involving safety net clinics. BMC health services research, 17(1), p.411.
- dailymail.co.uk 2019, Almost 20% of patients waiting for a hip replacement on the NHS are suffering pain they consider to be 'worse than DEATH', Available at: https://www.dailymail.co.uk/health/article-7360437/20-patients-waiting-hip-replacement-suffering-pain-worse-DEATH.html [Accessed on: 27th December 2019]
- dailymail.co.uk 2019, NHS waiting lists are at an all-time high with 4.41MILLION people in England awaiting a procedure and more than half a million have waited four months or more, Available at: https://www.dailymail.co.uk/health/article-7558509/NHS-crisis-Waiting-list-routine-ops-hits-record-high-4-41million.html [Accessed on: 26th December 2019]
- Deeny, S.R. and Steventon, A., 2015. Making sense of the shadows: priorities for creating a learning healthcare system based on routinely collected data. BMJ Qual Saf, 24(8), pp.505-515.
- Ellis, P. and Abbott, J., 2018. Applying Lewin's change model in the kidney care unit: unfreezing. Journal of Kidney Care, 3(4), pp.259-261.
- england.nhs.uk 2014, Change is the key to NHS survival, Available at: https://www.england.nhs.uk/2014/03/nhs-survival/ [Accessed on: 29th December 2019]
- Foronda, C., MacWilliams, B. and McArthur, E., 2016. Interprofessional communication in healthcare: An integrative review. Nurse education in practice, 19, pp.36-40.
- gov.uk 2011, National Patient Safety Agency (NPSA), Available at: https://www.gov.uk/government/organisations/national-patient-safety-agency [Accessed on: 29th December 2019]
- Halligan, A., 2013. The Francis report: what you permit, you promote. Journal of the Royal Society of Medicine, 106(4), p.116.
- Hardcastle, S.J. and Hagger, M.S., 2016. Psychographic profiling for effective health behavior change interventions. Frontiers in Psychology, 6, p.1988.
- healthwatch.co.uk 2019, Healhwatch England: What do we do?, Available at: https://www.healthwatch.co.uk/what-we-do [Accessed on: 28th December 2019]
- Hut-Mossel, L., Welker, G., Ahaus, K. and Gans, R., 2017. Understanding how and why audits work: protocol for a realist review of audit programmes to improve hospital care. BMJ open, 7(6), p.e015121.
- Johnson, M.J. and May, C.R., 2015. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ open, 5(9), p.e008592.
- Khayal, I.S. and Farid, A.M., 2018. Architecting a system model for personalized healthcare delivery and managed individual health outcomes. Complexity, 2018. pp.20-34.
- kingsfund.org.uk 2016, Readiness to change in NHS organisations, Available at: https://www.kingsfund.org.uk/blog/2016/04/readiness-to-change [Accessed on: 28th December 2019]
- Kuo, Y.L. and Chen, I.J., 2019. Facilitating a change model in age-friendly hospital certification: Strategies and effects. PloS one, 14(4), p.e0213496.
- Leis, J.A. and Shojania, K.G., 2017. A primer on PDSA: executing plan–do–study–act cycles in practice, not just in name. BMJ Qual Saf, 26(7), pp.572-577.
- Lestander, Ö., Lehto, N. and Engström, Å., 2016. Nursing students' perceptions of learning after high fidelity simulation: effects of a three-step post-simulation reflection model. Nurse education today, 40, pp.219-224.
- Mahanta, T.G., Boruah, M., Singh, V.K., Gogoi, P., Rane, T. and Mahanta, B.N., 2016. Effect of social and behavior change communication by using infotainment in community perception of adolescent girls for reproductive and sexual health care in high priority districts of Assam. Clinical Epidemiology and Global Health, 4(3), pp.133-139.
- Mazzocato, P., Stenfors-Hayes, T., von Thiele Schwarz, U., Hasson, H. and Nyström, M.E., 2016. Kaizen practice in healthcare: a qualitative analysis of hospital employees' suggestions for improvement. BMJ open, 6(7), p.e012256.
- McCaffrey, R. and Reinoso, H., 2017. Transformational leadership: A model for advanced practice holistic nurses. Journal of holistic nursing, 35(4), pp.397-404.
- McCaffrey, R. and Reinoso, H., 2017. Transformational leadership: A model for advanced practice holistic nurses. Journal of holistic nursing, 35(4), pp.397-404.
- Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M. and Wolf, A., 2017. Barriers and facilitators to the implementation of person‐centred care in different healthcare contexts. Scandinavian journal of caring sciences, 31(4), pp.662-673.
- Moro Visconti, R., 2016. Healthcare public-private partnerships in Italy: Assessing risk sharing and governance issues with PESTLE and SWOT analysis. Corporate Ownership and Control, 13(4). pp.20-34.
- Murphy, K., Chuma, T., Mathews, C., Steyn, K. and Levitt, N., 2015. A qualitative study of the experiences of care and motivation for effective self-management among diabetic and hypertensive patients attending public sector primary health care services in South Africa. BMC health services research, 15(1), p.303.
- nice.org.uk 2019, National Institute of Health and Care Excellence: About, Available at: https://www.nice.org.uk/about [Accessed on: 28th December 2019]
- nice.org.uk 2019, National Institute of Health and Care Excellence: About, Available at: https://www.nice.org.uk/about [Accessed on: 28th December 2019]
- Oueida, S., Aloqaily, M. and Ionescu, S., 2019. A smart healthcare reward model for resource allocation in smart city. Multimedia Tools and Applications, 78(17), pp.24573-24594.
- Parker, S.G., Downes, T., Godfrey, M., Matthews, R. and Martin, F.C., 2018. Age and Ageing to introduce a new category of paper: healthcare improvement science. Age and ageing, 48(2), pp.178-184.
- Purushotham, S., Meng, C., Che, Z. and Liu, Y., 2018. Benchmarking deep learning models on large healthcare datasets. Journal of biomedical informatics, 83, pp.112-134.
- Reed, J.E. and Card, A.J., 2016. The problem with plan-do-study-act cycles. BMJ Qual Saf, 25(3), pp.147-152.
- Reichenpfader, U., Carlfjord, S. and Nilsen, P., 2015. Leadership in evidence-based practice: a systematic review. Leadership in Health Services, 28(4), pp.298-316.
- Selby, D., Seccaraccia, D., Huth, J., Kurppa, K. and Fitch, M., 2017. Patient versus health care provider perspectives on spirituality and spiritual care: the potential to miss the moment. Annals of palliative medicine, 6(2), pp.143-152.
- Sharma, S., Saeed, A., Johnson, C., Gadegaard, N. and Cass, A.E., 2017. Rapid, low cost prototyping of transdermal devices for personal healthcare monitoring. Sensing and Bio-Sensing Research, 13, pp.104-108.
- Stonehouse, D., 2019. Reflection and you. British Journal of Healthcare Assistants, 13(4), pp.182-184.
- telegraph.co.uk 2015, Quality of NHS care is 'poor to mediocre' compared to other developed nations, OECD warns, Available at: https://www.telegraph.co.uk/news/health/news/11974620/Quality-of-NHS-care-is-poor-to-mediocre-compared-to-other-developed-nations-OECD-warns.html [Accessed on: 29th December 2019]
- Thomson III, N.B., Rawson, J.V., Slade, C.P. and Bledsoe, M., 2016. Transformation and Transformational Leadership:: A Review of the Current and Relevant Literature for Academic Radiologists. Academic radiology, 23(5), pp.592-599.
- Willis, C.D., Saul, J., Bevan, H., Scheirer, M.A., Best, A., Greenhalgh, T., Mannion, R., Cornelissen, E., Howland, D., Jenkins, E. and Bitz, J., 2016. Sustaining organizational culture change in health systems. Journal of health organization and management, 30(1), pp.2-30.
- Wright, M.C. and Endsley, M.R., 2017. Building shared situation awareness in healthcare settings. In Improving healthcare team communication (pp. 97-114). CRC Press.
Take a deeper dive into A Critical Analysis of Relevant Literature with our additional resources.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



