Assessment And Management of Lower
Introduction
Existing literatures on cellulitis indicate that it is a commonly occurring skin infection that also affects the subcutaneous tissues and may lead to life threatening health complications (Shatnawi et al, 2018). It is prevalently experienced in both emergency department and primary care settings with estimation that patients experiencing cellulitis are 1-14% of emergency room visits and 4-17% of patients admitted for various health problems including Medicare, drug users and HIV patients (Health & Social Care Information Centre 2019). This paper is particularly interested in the assessment and management of lower limb cellulitis because while its severity and clinical presentation varies among different patients, there seems to be a conflict in what physicians consider to be the best assessment and management pathway for it, a matter that may benefit from further exploration and healthcare dissertation help (Simonsen et al, 2006).
Defining Cellulitis
From time immemorial, cellulitis has been diagnosed as a bacterial infection that affects the skin and presents itself as an inflammation (Chakradeo et al, 2018). According to Vollazos et al (2018), inflammation is a body response to trauma that presents itself in the form of pain, redness, warmth or swelling. Nonetheless, from the evidence provided by Shatnawi et al (2018), we argue that inflammation associated with cellulitis may be quiet severe and may affect both the subcutaneous tissues and the skin, spreading to the lymph nodes through to the bloodstream. However, it is important to note that cellulitis can occur anywhere in the body, although it commonly occurs in the lower limbs especially at the legs near ankles and shins (Williams et al, 2014).
Apparently, Cellulitis occurs through an elaborate process that can be biologically explained. Dean & Saitiani (2013) explain that under normal circumstances, the skin has a mechanism for protecting the body from disease-causing microorganisms. Ideally, it occurs as the first line of protection that defends the body from the microorganisms. However, we argue that the bacterial infection occurs when the bacteria manage to penetrate the skin through wounds or abrasions on the skin surface, as well as through any existing leg condition (e.g. athletes’ foot) that exposes the skin (Ferri & Ferri, 2019). While one may argue that the skin usually protects the body from such infections, there are some kind of patients (e.g. those with burns, surgical-related infections, or diabetes) who are at high risk of the bacterial infection and therefore the bacteria gets to multiply faster in their body. This multiplication triggers an immune response that is characterized by an inflammatory response thereby resulting in lower limb Cellulitis (Goel & Goel, 2016).
Incidence/Prevalence of Cellulitis
There is a paucity of research evidence highlighting current prevalence levels of cellulitis in the UK and world over. However, latest statistics by Health & Social Care Information Centre (2019) indicate that between 2013 -2014, 104,598 cases of cellulitis were reported to have been treated in secondary care in the UK; 69,229 among them being hospital admissions that occupied an average bed stay duration of 6.2 days (NHS Institute of Innovation and Improvement, 2019). However, according to NHS Institute of Innovation and Improvement (2019), these figures might be higher because most of cellulitis cases are also treated in primary care. Nonetheless, it is estimated that in 2013-2014, the mean age admitted for cellulitis was at 63 years, while 36.5% were aged 75 years or above.

Systemic and Local Predisposing Factors for Lower Limb Cellulitis
Several research studies have attempted to evaluate the systemic and local predisposing risk factors for lower limb cellulitis and yielded mixed results. For instance the study by Sigrídur (2005) a history of saphenectomy and previous cellulitis are risk factors for toe webs or leg lesions infected by pathogens are potential entry points of organisms that cause lower limb cellulitis. However, when the researchers excluded toe web bacterial infections from the analysis, toe web dermatophytosis did not appearand this indicates that bacterial pathogens colonization of toe webs is more strongly associated with lower limb cellulitis than its fungal infection. Significantly though, one limitation of these findings is that the study was conducted almost 10 years ago, an d thus may not be a current evidence to support practice. Against that backdrop, we argue based on the research by Gawkrodger et al (2012) that people with disrupted areas of the skin, or those with trauma are more predisposed to cellulitis, as well as those with other medical conditions such as chronic leg ulcers, and those experiencing leg wounds colonized by Pseudomonas, streptococci, staphylococci and Bacteroides spp, or other less common types of bacteria. Perhaps the closest and latest study on risk factors for lower limb cellulitis, Quirke et al (2016) conducted systematic literature review to evaluate various controlled observational studies that have explored the risk factors for non-purulent cellulitis of the lower limb. Whereas diabetes was underrepresented among the reviewed studies, the study found that local risk factors (e.g. wounds, edema, ulcers, and skin breakdown and leg wounds) played more role as risk factors for the disease than systematic risk factors (e.g. diabetes). Hence, based on this research evidence, we argue that clinicians should consider treating local predisposing factors while also giving adequate attention to systemic risk factors.
Symptoms of Lower Limb Cellulitis
The commonly known symptoms of Cellulitis is skin discoloration and changes in temperature, and this may include swelling on the lower leg and can also begin from the calf; raised glossy skin appearance, pale skin and red skin with a clear demarcation of both, skin redness and tenderness or pain, increased white cell count, and leaking of yellow fluid from the skin (Buck, 2011). According to Bennet et al (2011), victims may also experience small red dots appearing on top of the Cellulitis, while in rare cases, the victim may experience small blisters. Weedon (2009) writes that ascending Cellulitis, a type of Cellulitis which extends up the legs, is usually caused by a staphylococcal or streptococcal infection, and typically starts from the foot with signs of swellings and tenderness with a calf around the wound site. The bacteria usually enter through a wound, which is usually the start of the infection. While it is extremely uncommon, a patient may experience a bilateral infection, which normally occurs when the bacteria enter through more than one wound (Fitzpatrick & Kang, 2019). Nonetheless, based on the evidence by Tsi Njim et al (2017), we argue that the toe web maceration is usually the commonest point of entry of the bacteria and this is usually because of tinea pedis. However, we observe that there are other conditions associated with the lower limbs that may be confused with Cellulitis. For instance, evidence by Katrina Chakradeo et al (2018) indicate that that one of the reasons why Cellulitis is challenging to diagnose is the fact that it can be confused by with other inflammations that occur as part of other diseases or as part of trauma processes. Based on this, we recommend that it is important to clearly identify the lower limb Cellulitis
because it might be confused with other arterial or venous diseases, as well as conditions related to cardiac failure because ideally, there are many conditions presenting in the lower limb that have common presenting features (e.g. tenderness, redness, and swelling). Hence, as Beyaratne et al (2018) argue, it may be more difficult for clinicians to identify Cellulitis by its presenting symptoms alone, and thus the need to use the spreading erythema as an accurate indicator of Cellulitis alongside other common presenting symptoms such as increased pain levels and temperature. Having said so, some symptoms similar to those of Cellulitis may emerge as a result of deep vein thrombosis (DVT) or chronic oedema. However, considering the assertions by Njim et al (2017), DVT is characterized by swollen legs and below the thrombus cyanotic, accompanied by some pain in the calf or dorsiflexed foot. Another source of diagnostic confusion is increased oedema among the elderly obese characterised by a significantly increased erythema. In this regard, Shatnawi et al (2018) claim that whereas this oedema may be prominent, it is usually symmetrical and not hot to touch. On the other hand, Cellulitis-related erythema is characterised by fever or local tenderness and this is usually a comparison point between other causes of leg swelling and lower limb Cellulitis. Shatnawi et al (2018) also observes that cellulitis may be confused with erysipelas, which is an infection that occurs in the superficial tissues and presents itself in large and painful blisters. Nonetheless, based on evidence by Shatnawi et al (2018), we present that there is a need to differentiate cellulitis, a condition that emerges as a secondary proceeding to eczema as the commonest disease that emerges in cases of staphylococcal. On the other hand, cellulitis secondary to preceding leg ulceration can be as a result of various bacterial organisms (Tianyi et al, 2018). Besides, we also acknowledge that leg ulcer patients may also
develop allergic contact dermatitis that are often caused by the application of creams, lotions, and dressings containing allergens (Shatnawi et al, 2018). Having evaluated various clinical presentations that may be confused with cellulitis, it is also important to note that these presentations have different diagnoses and are treated differently, besides having different levels of long-term significance, making it important to differentiate the from cellulitis being dealt with (Shatnawi et al, 2018). In most cases, according to Gawkrodger et al (2012), practitioners are advised to seek expert opinion if they have any doubts while diagnosing cellulitis.
Varicose Eczema
Njim et al (2017) define varicose eczema as one of the commonest inflammatory dermatosis that affects the lower limbs and is often associated with varicose veins in terms of coexistence. Some of the most common symptoms of varicose eczema include scaling, pigmentation, crusting skin, tight red skin tissues, and pigmentation (Tianyi et al, 2018). Besides, patients with varicose eczema may present venous stasis eczema which is a secondary infection of varicose eczema and may present symptoms such as itching, yellow crusting, weeping. According to Beyaratne et al (2018) these symptoms may require antibiotics, or if the infection is diagnosed, an antimicrobial emollient may be required.
Athlete’s Foot
This is another type of lower limb cellulitis but is not commonly diagnosed in other clinical areas apart from dermatology (Tianyi et al, 2018). According to Gawkrodger et al (2012), it presents itself in the form of maceration, scaling, erythema of fissuring especially in the interdigital area. Interestingly, treatment and diagnosis of athlete’s foot can reduce the chances of recurrent cellulitis (Dean & Saitiani 2013).
Assessment and Diagnosis of Cellulitis
he complex nature of cellulitis assessment has led to the development of various techniques an procedures used by practitioners to guide in conducting the assessment. Gawkrodger et al (2012) says that whatever the cause of cellulitis, it is important for practitioners to refer to an algorithm that helps to develop a primary and secondary case treatment with effective guidance to the correct choice of treatment. Medical history is among the most important procedures in the assessment and diagnosis of cellulitis. Gawkrodger et al (2012) argue that in doing so, the practitioner should define the onset of symptoms as well as the starting point of the inflammation while the history of any form of trauma should be ascertained to ensure the best antibiotic is prescribed. Whereas injury might have occurred several periods before infection, Dean & Saitiani (2013) observe that only a few patients associate the onset to such injuries. In fact, these injuries may be associated to environments with a high risk of contamination; for instance cuts and wounds experienced in water environments such as lakes or rivers, because the waters may have been contaminated with bacteria (Tianyi et al 2018). Hence, we argue that the diagnosing practitioner should consider water-borne bacteria if the patient is not responding to conventional antibiotics. Dean & Saitiani (2013) say that while diagnosing lower limb cellulitis, it is important to note that the skin changes might be accompanied by malaise, shivering, nausea, and fever. However, Tianyi et al (2018) argues that when the patient is developing progressive symptoms, then the
practitioner can suspect a deeper or more acute infection such as fasciitis, and thus the need for acute care. On the other hand, Shatnawi et al (2018) writes that cellulitis that has spread to adjacent body structure such as the blood should be treated with emergency; and requires immediate hospital admission, while those with mild cellulitis without any systemically presenting symptoms can be managed by primary care.
Management of Cellulitis
Dean & Saitiani (2013) point out that upon assessing and diagnosing lower limb cellulitis, treatment depends on whether it is dry or wet, as well as the causative agent. However, we argue that in both cases, the patient will require systematic antibiotic therapy. Nevertheless, based on evidence by Gawkrodger et al (2012), we infer that lower limb cellulitis is commonly treated with a combination of benzylpenicillin and various types of an antibiotic such as flucloxacillin. Besides, we recommend that the antibiotics can first be given intravenously then later administered orally after they have taken effect (Njim et al, 2017).
Tianyi et al (2018) observes that whereas most patients may respond positively to the antibiotics, a few cases may not be responsive and this could be as a result of drug resistance, or the need for an antibiotic combination. On the other hand, if the patient presents erosions, crusts or any pustules, there may be a need for a swab for culture especially if the patient has failed to respond to first-line oral antibiotic (Goel & Goel, 2016). A blood cell count may reveal leucocytosis. In this regard, the practitioner would need to conduct a blood culture especially of the patient is very unwell or is presenting high fevers. In other cases of severe infection, the physician would need to conduct an elevation of the patient’s C - reactive protein level and erythrocyte sedimentation rate. However, in doing so, Dean &
Saitiani (2013) recommend that there should be a recording of the basement observations such as blood pressure, pulse, and respiration. But lower limb cellulitis has been associated with many complications, characterized by long-term morbidity, creating the need for a quick and vigorous treatment Beyaratne et al (2018). When the redness extends and the symptoms become more severe, there may be more serious infections in the inner skin (Tianyi et al, 2018). Worryingly, Dean & Saitiani (2013) acknowledge that once the bacteria enter the inner layers of the skin, they can spread easily and enter the bloodstream. When the streptococcal infection spreads into the deeper layers of the fascial lining, the patient may develop necrotizing fasciitis, a condition that requires an urgent hospitalization and treatment (Beyaratne et al 2018).
In most cases, according to Shatnawi et al (2018), anaerobes and streptococci are the causative agents of necrotizing fasciitis – a condition that first resembles dusky cellulitis but later turns into extending necrosis of the subcutaneous tissue and the skin. Nonetheless, based on the evidence by highlight further that despite systemic antibiotics and early surgical debridement, its prognosis is often poor (Njim et al, 2017). When a patient experiences recurring cellulitis, they may later experience lymphangitis – if left untreated, can lead to lymphoedema (Goel & Goel, 2016). It is therefore important to treat these symptoms early enough and if there is a continual reoccurrence of cellulitis, the practitioner should consider a long-term penicillin treatment. Long-term treatment would also include an emollient moisturizing for several weeks so as to return the skin to its normal elasticity (Goel & Goel, 2016). On the other hand, we also recommend that the patient should be encouraged to maintain good skin care to reduce the risk.
While the scarring continues to face, it is important to stay away from trauma or the sun to ensure that the new skin remains unexposed to any vulnerabilities. If the patient is experiencing cellulitis as a secondary condition to ulceration or venous disease, they may need to undergo compression therapy. Nevertheless, the full treatment for venous ulceration and venous disease include a holistic assessment, which includes a proper dressing based on the needs of the current wound, hosiery of bandaging, elevation of the lower limb, patient education (based on the agreed treatment plan) and proper nutrition (Shatnawi et al, 2018). We argue that when treating cellulitis a keen consideration should be given to patients with soft tissue infections such as carbuncles because such collections should be drained (Goel & Goel, 2016). Moreover, according to Beyaratne et al (2018), the collections should be subjected to bacterial culture while considering systemic antibiotics in patients’ shoe signs of infection are systemic.
On the other hand, systemic antimicrobials are recommended for patients with non-purulent skin (Njim et al, 2017). Similarly, Shatnawi et al (2018) states that patients with no systemic signs of infection and no comorbidities (i.e. Dundee Class I) are recommendable for oral antimicrobial therapy, while some Dandee Class II patients may be recommendable for an initial period of intravenous therapy in the hospital or through outpatient antimicrobial therapy. However, Goel & Goel, (2016) opine that the intravenous agents are good for patients showing evidence of systemic infection as well as those who do not show any response to initial oral therapy. Important to note though, patients who show signs of deep necrotizing infection should urgently be admitted for surgical debridement and inspection.
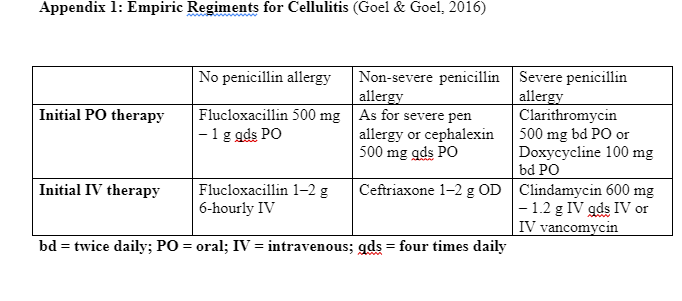
While the local resistance rate and practice may dictate the recommendable antimicrobial agent based, the suggested empiric regiments are outlined in Appendix (1). However, patients with infections associated with animal or human bites may need to undergo a broader spectrum of antimicrobial treatment and this is subject to discussion with an infection specialist (Goel & Goel, 2016). The same should apply in cases where cellulitis is appearing on atypical positions such as an upper limb, face or torso. According to Njim et al (2017), patients with necrotizing or severe infections would be subjected to an initial antimicrobial cover including streptococci, staphylococci, and Gram-organisms, as well as an agent with anti-toxin production such as linezolid. On the other hand, patients with a history of, or predisposed to Methicillin-resistant Staphylococcus aureus (MRSA) should be treated with an active agent against methicillin-resistant (MRSA). However, it is important to note that recent trials conducted in the USA reveal that the use of agent active against MRSA may not be effective in treating non-purulent cellulitis (Pallin et al, 2013).
Prophylaxis
Goel & Goel (2016) write that patients with a history of lower limbs cellulitis have an 8-20% chance of recurrence. According to Shatnawi et al (2018), such patients should be subjected to a careful evaluation to identify any predisposing factors such as lymphoedema, lower limb edema tunea pedis, or dermatitis. On the other hand, Goel & Goel (2016) argues that patients who have experienced three or four episodes of cellulitis in a year regardless of having addressed the predisposing factors should be considered for prophylactic antimicrobial therapy, especially if those symptoms persist (Stevens et al 2014).
Enhancing Cellulitis Service
According to CREST (2005) guidelines, there should be an increased awareness to improve cellulitis management and diagnosis both at acute and primary care levels. CREST (2005) also showed dedication towards the delivery of cellulitis services to ensure reduced delays in diagnosis, reduce costs of treatment and to enhance education on cellulitis through a multidisciplinary approach. CREST proposes that the multidisciplinary approach should include nurses, pharmacists, physiotherapists, GPs, microbiologists and dermatologists. Indeed, CREST acknowledges that there are some hospital trusts such as the Norfolk and Norwich University Hospital in the UK has shown a great interest in deriving the initiative of delivery of cellulitis services by offering a same-day referral cellulitis clinic in the dermatology outpatient department, where patients with lower limb cellulitis are referred to receive thorough assessment such as diagnosis, investigation, treatment and any other differential diagnosis that is associated with skin disease.

Continue your journey with our comprehensive guide to Assessment and Care Plan for Mr John.
References
- Buck, C. J. (2011). ICD-10-CM, Standard Edition DRAFT - E-Book.
- Bennett, J. E., In Dolin, R., & In Mandell, G. L. (2011). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Edinburgh: Saunders/Elsevier.
- Beyaratne, D. D. K., Liyanapathirana, C., Fonseka, C. L., & Wijekoon, P. W. M. C. S. B. (2018). A Rare Case of Eosinophilic Granulomatosis with Polyangiitis Associated with Cryoglobulinemia Presenting with a Bullous Skin Eruption of the Lower Limbs. Case Reports in Medicine.
- Chakradeo, K., Paul Chia, Y. Y., Liu, C., Mudge, D. W., & De Silva, J. (2018). Disseminated cryptococcosis presenting initially as lower limb cellulitis in a renal transplant recipient - a case report. BMC Nephrology, 19, 1.
- Collazos, J., de la Fuente, B., Garcia, A., Gomez, H., Menendez, C., Enriquez, H., … Asensi, V. (2018). Cellulitis in adult patients: A large, multicenter, observational, prospective study of 606 episodes and analysis of the factors related to the response to treatment. PLoS ONE, (9).
- CREST (2005) Guidelines on the management of cellulitis in adults.
- Dean, S., & Satiani, B. (2013). Color Atlas and Synopsis of Vascular Disease. Blacklick: McGraw-Hill Publishing. Ferri, F. F., & Ferri, F. F. (2019). Ferri's clinical advisor 2019: 5 books in 1. Philadelphia, PA : Elsevier.
- Fitzpatrick, T. B., & Kang, S. (2019). Fitzpatrick's dermatology. New York : McGraw-Hill Education. Goel, T. C., & Goel, A. (2016). Lymphatic filariasis. Singapore : Springer, 2016. Gawkrodger, D., & Ardern-Jones, M. R. (2012). Dermatology E-Book: An Illustrated Colour Text. Health & Social Care Information Centre (2019) Hospital Episodes Statistics: https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics
- Katrina Chakradeo, Y. Y. Paul Chia, Cheng Liu, David W. Mudge, & Janath De Silva. (2018). Disseminated cryptococcosis presenting initially as lower limb cellulitis in a renal transplant recipient – a case report. BMC Nephrology, (1), 1.
- Njim, T., Aminde, L. N., Agbor, V. N., Toukam, L. D., Kashaf, S. S., & Ohuma, E. O. (2017). Risk factors of lower limb cellulitis in a level-two healthcare facility in Cameroon: a case-control study. BMC Infectious Diseases, (1).
- Njim, T., Aminde, L. N., Agbor, V. N., Toukam, L. D., Kashaf, S. S., & Ohuma, E. O. (2017). Risk factors of lower limb cellulitis in a level-two healthcare facility in Cameroon: a case-control study. BMC Infectious Diseases, (1).
- Pallin J. Binder D. Allen B, et al. (2013) Clinical trial: comparative effectiveness of cephalexin plus trimethoprim-sulfamethoxazole versus cephalexin alone for treatment of uncomplicated cellulitis: a randomized controlled trial. Clin Infect Dis. 2013;56:1754–62.
- Quirke M., Ayoub F., McCabe A., Boland F., Smith B., O'Sullivan R., Wakai A. (2017) Risk factors for nonpurulent leg cellulitis: a systematic review and meta‐analysis, British Journal of Dermatology, Volume177 (2).
- Stevens L. Bisno L. Chambers F, et al. (2014) Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10–52.
- Shatnawi, N. J., Al-Zoubi, N. A., Hawamdeh, H. M., Khader, Y. S., Garaibeh, K., & Heis, H. A. (2018). Predictors of major lower limb amputation in type 2 diabetic patients referred for hospital care with diabetic foot syndrome. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 313.
- Simonsen E., Orman V., Hatch E., Jones S., Gren L., , Hegmann T., And Lyon L. (2006) Cellulitis incidence in a defined population Epidemiol Infect. Apr; 134(2): 293–299.
- Sigrídur B, Magnús G, Anna S., Gunnar B., Hugrún R., Már K., Ingibjörg H. (2005) Risk Factors for Acute Cellulitis of the Lower Limb: A Prospective Case-Control Study, Clinical Infectious Diseases, Volume 41, Issue 10, 15 November, Pages 1416–1422.
- Tianyi, F.-L., Mbanga, C. M., Danwang, C., & Agbor, V. N. (2018). Risk factors and complications of lower limb cellulitis in Africa: a systematic review. BMJ Open, 8(7), 1. Tsi Njim, Leopold Ndemnge Aminde, Valirie Ndip Agbor, Louise Daniele Toukam, Sara Saheb Kashaf, & Eric O. Ohuma. (2017). Risk factors of lower limb cellulitis in a level-two healthcare facility in Cameroon: a case-control study. BMC Infectious Diseases, (1), 1.
- Williams, H., Bigby, M., Diepgen, T., Herxheimer, A., Naldi, L., & Rzany, B. (2014). Evidence-Based Dermatology. John Wiley & Sons. Weedon, D. (2009). Weedon's Skin Pathology E-Book: Expert Consult - Online and Print.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



