Care Planning in Health Services
Introduction:
Care planning is the process in which health professionals discuss, analyse and review an action plan in order to achieve the behavioural, psychological and physical transformation of patients. This assignment is going to discuss the stages of the care delivery process. Moreover, this study will also identify the legislation that is relevant to care planning. This assignment will determine the ranges of information that is inevitable to make the proper assessment by using the observation and communication skill. Additionally, for those pursuing related research, healthcare dissertation help can provide valuable insights. Moreover, this study will discuss how care providers involve service users in care planning, in order to implement the anti-discriminatory process into practice. Finally, this study will demonstrate the multi-professional working process in care planning in order to provide optimum care and support to service users.
Identify the relevant legislation in relation to care planning and stages of care delivery process in health and social care: (LO1)
Legislations and policy in relation to care planning process:
Different legislations are associated with the delivery of compassionate care to service users. Under the Health and Social Care Act 2010, NHS nurse and service providers would focus on the quality and outcomes management in the care delivery process (NHS, 2019). Quality patient care and outcomes lay the foundation for effective care delivery system. UK Policy for Health and Social Care sets principles for conducting effective care delivery process. The principle protect and promote the interest of the service users, patient and public in health and social care context, by conducting the proper quality management, effective care delivery process and proper assessment (Gibson et al. 2015). Under the Health and Social Care Act 2010 the entire professional associated with the health bodies such as Department of Health, Clinical Commissioning Group, NHS England and Public Health England, would promote equal care and optimum support to the service uses. Under the Equality Act 2010, NHS nurses and staffs would promote equality in care delivery process, in which service user provided with the best care and support irrespective of their gender, ethnicity, race, religion and caste. On the contrary Gammie et al. (2015) argued that sometimes healthcare professions are unable to provide the equal care and support to service users due to different case and reason of their illness, which needs specific treatment process. Under Workforce Disability Equality Standard (WDES) set by Department of Health UK, healthcare professions need to set the specific measurements in order to analyse the level of disability of the disabled staffs. Based on the guidelines of Disability Discrimination Act (1995), health and social care staffs would focus on the special needs of the disabled patient and set the specific care recess that will assist them to promote health and wellbeing of the disabled person. Under the Equality Act 2010, in order to provide the care process to service users suffering from certain kind of disability, the service providers and health professionals would focus on protecting the patient from any kind of discrimination and bias. As stated by Moaddab et al. (2015), people with mental illness such as depression, dementia, schizophrenia and obsessive-compulsive disorders would be facilitative with such as care process, in which health professionals can be able to access day-to-day inspection of health.

Stages and design of care delivery process in health and social care:
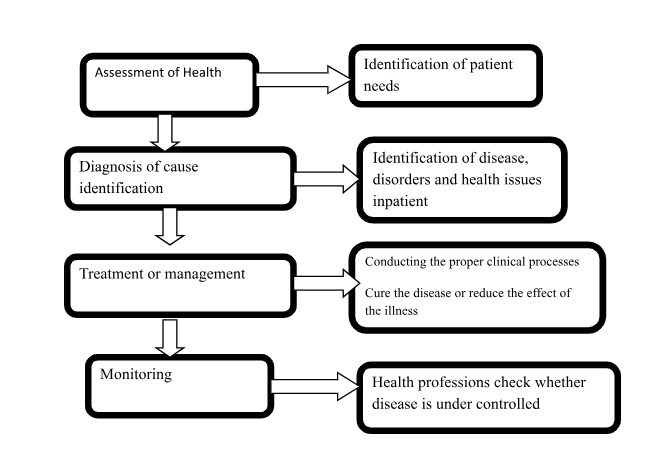
Professional care and optimal health need acknowledged designs or methods of proper care delivery process in order to access, analyse and address the health issues (Weled et al. 2015). Proper care delivery process is associated not only with identification and assessment if the health care issues but also is associated with conducting proper clinical setting in order to eliminate the health issues for promoting health and wellbeing of the service users. Based on the NHS guidelines each care delivery process would have four common stages such as recognition or assessment, diagnosis or cause identification, treatment or management, and monitoring.
1. Recognition or assessment:
A healthcare assessment is primary stage of a care process which concerns with identification of patient needs and the process of addressing these needs in an effective manner (Aarons et al. 2017). National Health Service (NHS) and Public Health England, set guidelines for conducting the high-quality healthcare system and high-skilled nursing facility in order to address the patient’s needs. In these stages, health professional performs the physical examination and tests in order to evaluate the current health status of the patient. As stated by Jenkins et al. (2015), though health assessment it is possible for healthcare professionals to determine any kind of disuse or health disorders in patients.
2. Diagnosis of cause identification:
This is the most important stages in a care delivery process, which is associated with identification of disease, disorders and health issues in patient by conducting the clinical examination of the symptoms and signs, evaluation of the test results and analysis of the patient's health history (Kim et al. 2017). Diagnosis is a process of finding out the cause of the current health issues and disease in the patient. NHS professions prescribed the relevant tests in order to determine the possible illness of patients. As stated by Jenkins et al. (2015), in some of the causes, an only physical test is not sufficient in order to determine the degree of development of illness. Health professionals use the diagnosis not only to determine the cause of the disease but also measure the severity of illness such as its possibility of regression, current stages of the disease and its progression. Based on the diagnosis, the overall clinical setting is developed in order to stop the progression of the disease.
3. Treatment or management
Treatment and management of the disease are associated with conducting the proper clinical processes which are able to cure the disease or reduce the effect of the illness (Jutkowit et al. 2016). Health professionals use medicines, surgeries, therapies and other possible treatment in order to cure the disease. In these stages, health professionals implement the better clinical strategies that they developed through the analysis of the health issues and causes of illness at the second stage of the care process, the diagnosis and cause identification. On the contrary Kim et al. (2017) argued that, in some cases, it is not possible for healthcare professionals to cure the disease. For example, in case of Diabetes and Hepatitis B, it is not possible for the doctors to cure the illness, but health professionals can use medicines and therapies in order to reduce the effects of this illness. National Institute for Health Care and Excellence (NICE), has set strategies for delivering the high-quality treatment process to all the UK based citizen, irrespective of their caste, religion, race and ethnicity. Moreover, NHS staffs provide free health check-up for UK based citizens such as BP and body temperature check up and measurement of blood sugar.
4. Monitoring:
Monitoring is the last stages in the care process, in which the health professions check whether disease is under controlled. As stated by Aarons et al. (2017), in case of chronic disease such as diabetes they cannot be controlled through the treatment process. In which aspect health professionals prescribe approved medicines and therapies in order to reduce the effected of illness onto the patient. Monitoring process assists the health professionals to analyse the result and outcomes of the applied treatment process. Through monitoring of the current health status if patient, health professional understand whether the treatment process is useful for the patient. If the patient is unable to respond properly to the treatment, then health professionals need to change the entire treatment process.
Identify the ranges of information that is required for appropriate needs assessment and demonstrate the use of observation and communication skill: (LO2)
Needs assessment is one of the important processes in healthcare:
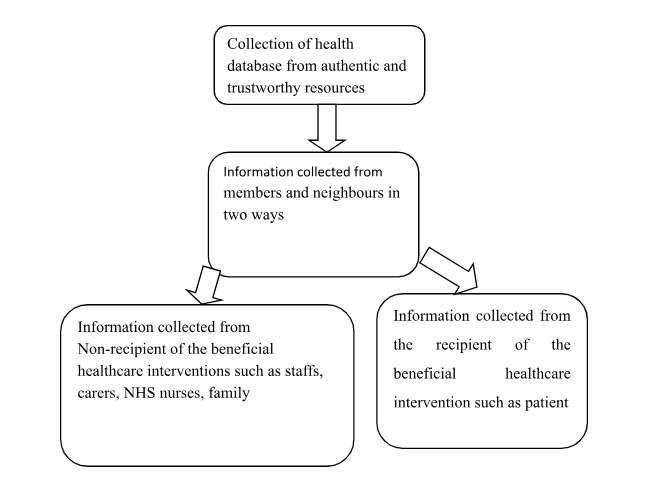
Need assessment is the process, in which the health professional gather the important information that is required for bringing about potential and effective changes in the healthcare process (Etkind et al. 2017). For conducting effective need assessment in healthcare, professions use relevant information that they have to collect from authentic and trustworthy resources. The resource that provides the proper information regarding conducting the proper need assessment are as follows:
Non-recipient of the beneficial healthcare interventions such as staffs, carers, NHS nurses, family members and neighbours.
Recipient of the beneficial healthcare intervention such as patient
Moreover, to collect the proper information regarding the health status of patient, doctors focus on the previous health cases of the patient. Through using the observation and proper communication skill, the healthcare professionals gather relevant database from the patient families and neighbours regarding the current health status and previous health complications of the patient. As stated by Cheung et al. (2017), different patient and service users have different needs which require specific observation process. In order to assess the different needs of the patient, health professional need to focus on conducting the proper comparison between the previous and current health status of the patient. In case of a patient with mental and physical disabilities, verbal communication skill is not enough for the health professional to gather relevant information regarding the heath stated of the patient. In this aspect, non-verbal communication process, is helpful, in order to determine the actual health needs of each patient by communicating with them in sign language.
Through conducting proper observation and monitoring process, health professionals are able to understand whether the needs can be met by developing proper clinical setting, in terms of dealing with the chronic illness, such as diabetes and cardiovascular disease, observation, monitoring and screening process are not helpful for gathering the relevant information about cause of illness. Moreover, health professional is unable to cure these disorders properly. In which aspect, needs assessment and observation is conducted in order to understand whether the disease can be controlled through the medicine. In the case of conducting the proper observation of the overall health status of the patient, health professional also gathers the possible information about the health issues and degree or severity of the disease.
Demonstrating the knowledge of the involvement of service users in care planning proper in order to implement anti-discriminatory practice: (LO3)
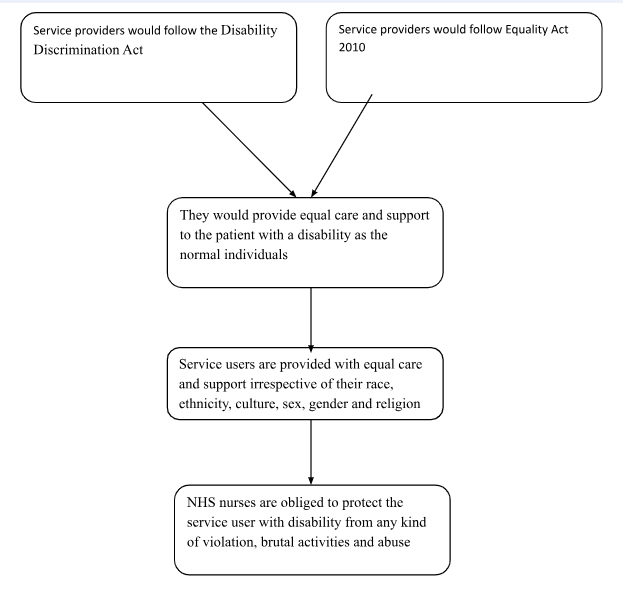
Involvement of service uses is important in the overall care process in order to maintain the quality and usefulness of the process. Under the Disability Discrimination Act service users with mental and physical disability would be provided with equal care and support as normal individuals. As stated by Fransen et al. (2017), health professions NHS staffs and Health Service Executives (HSE), would ensure that service users are provided with equal care and support irrespective of their race, ethnicity, culture, sex, gender and religion. Moreover, NHS set guidelines in order to implement the anti-discriminatory practice in the healthcare, in which all NHS staffs and professional would ensure that opinion and decision of service users would be listening in proper manner (Liff and Wikström, 2015). Moreover, NICE sets principles in order to work in partnership with the service in healthcare in which all the staffs and healthcare professional would provide respect and dignity to each service users. Healthcare staffs and NHS nurses are obliged to protect the service user with disability from any kind of violation, brutal activities and abuse. Moreover, all the service users would be involved in the care process to get clear information about their health, safety and care process. As stated by Fransen et al. (2015), NHS staffs act as health education executives, who provide proper education to each service user regarding the management of their own health, wellbeing and safety.
Importance of multi-professional working process: (LO4)
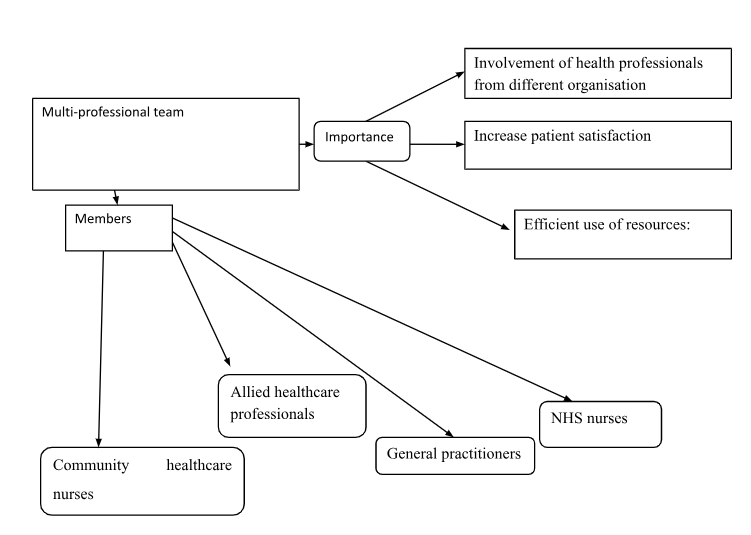
Multidisciplinary or multi-professional team convey several benefits to the patient as well as to the health professional working in a team. These benefits are as follows:
Involvement of health professionals from different organisation:
The multi-professions working process is important in health and social care in which different efficient healthcare professionals from different organisations work together. As stated by Fransen et al. (2017), this process allows the sharing of new thoughts, ideas and decisions in terms of providing high-quality compassionate care to service users. According to the NHS guidelines and NICE, the ideal multi-professional team includes the following professional such as
General practitioners
NHS nurses
Community healthcare nurses
Allied healthcare professionals (the mix of health care professional from the governmental and non-governmental organisation), which includes psychotherapists, dietician, psychologist, occupational therapist, social workers and the Aboriginal health workers
Health educators, for example, diabetes educators who provide effective knowledge to service users and the family about how to deal with diabetes in an effective manner.

Increase patient satisfaction:
Multi-professional team working process allows the healthcare professionals and staffs to provide compassionate care in order to improve the health outcomes of the patient. Through providing high-quality care, it is possible for the health professional to improve patient satisfaction. As stead by Liff and Wikström (2015), multi-professionals l team working process in health and social care assist the healthcare framework to gain innovative ideas and treatment process that is developed by the different healthcare professional of a different organisation. Moreover, shared knowledge and leadership process in the multi-professional working process assist the health professionals to make group discussion with colleges and superiors to the developed effective clinical setting in order to deal with the critical and chronic disease. Moreover, through the multi-professional working process, NHS staffs and allied healthcare professionals can form trustworthy and respectful relations between the service users and care providers. According to (0, through working in a multi-disciplinary group, there is a skill mix process in which the skills and knowledge of different professionals are shared and mix together in order to develop high-quality treatment process. National Institute for Healthcare and Excellence (NICE) has set the guidelines for multi-professional team in which the health care professionals need to focus on common organisational goal that is promoting the health and wellbeing of the service users. Moreover, through the multidisciplinary working process, it is possible for healthcare staffs to make agreed clinical governance framework.
Efficient use of resources:
Team members of multi-professional group are highly skilled and highly qualified individuals who can make proper usage of health and social care resources in order to meet the healthcare needs of service users (Husebø and Akerjordet, 2016). Moreover, a healthcare professional in the multi-professional team train the subordinate staffs on how to use different resources such as managing people, service users, different healthcare instruments, technical machines and different clinical apparatus. Moreover, in the multi-profession team, there are staffs from a diverse background which can use their individual skill in order to form effective strategies about to use the resources in a proper manner in order to provide the best care of the service users. Such as NHS staffs would focus on maintenance of each medical apparatus and the healthcare instruments in order to assure the safety of service users. Moreover, the healthcare professional would assure that all treatment process is selected for the patient based on their healthcare needs; the HR professions in the multi-professional group would focus on hiring and appointing eligible staffs and health professional in order to assure the high-class service delivery process.
Conclusion:
From the above-mentioned discussion, it can be concluded that the Department of Health, England, has set relevant policies and legislation in order to provide high-quality service delivery process. Based on these legislations such as Health and Social Care Act 2012, Equality Act 2010 and UK Public Healthcare Policy, healthcare professional needs to follow the Codes of Conduct and the Care standard in order to deliver the compassionate care process to the service user. Moreover, from the discussion, it can also be concluded that healthcare professionals need to follow the anti-discretionary legislation in order to protect service users from any kind of bias, discrimination and the abuse. Multi-professional working processes one of the most efficient health care frameworks, which assures that high skilled professional and staffs from different organisational work together in order to provide the best care to the service users.
Reference list:
Aarons, G.A., Sklar, M., Mustanski, B., Benbow, N. and Brown, C.H., 2017. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implementation Science, 12(1), p.111.
Benkedjouh, T., Medjaher, K., Zerhouni, N. and Rechak, S., 2015. Health assessment and life prediction of cutting tools based on support vector regression. Journal of Intelligent Manufacturing, 26(2), pp.213-223.
Cheung, K.L., Evers, S.M., de Vries, H. and Hiligsmann, M., 2017. Most important barriers and facilitators regarding the use of health technology assessment. International journal of technology assessment in health care, 33(2), pp.183-191.
Etkind, S.N., Bone, A.E., Gomes, B., Lovell, N., Evans, C.J., Higginson, I.J. and Murtagh, F.E.M., 2017. How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC Medicine, 15(1), p.102.
Fransen, A.F., Banga, F.R., van de Ven, J., Mol, B.W.J. and Oei, S.G., 2015. Multi‐professional simulation‐based team training in obstetric emergencies for improving patient outcomes and trainees' performance. Cochrane Database of Systematic Reviews, (2).
Fransen, A.F., Ven, J., Schuit, E., Tetering, A.A.C., Mol, B.W. and Oei, S.G., 2017. Simulation‐based team training for multi‐professional obstetric care teams to improve patient outcome: a multicentre, cluster randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology, 124(4), pp.641-650.
Gibson, T.B., Herring, S.A., Kutcher, J.S. and Broglio, S.P., 2015. Analyzing the effect of state legislation on health care utilization for children with concussion. JAMA pediatrics, 169(2), pp.163-168.
Husebø, S.E. and Akerjordet, K., 2016. Quantitative systematic review of multi‐professional teamwork and leadership training to optimize patient outcomes in acute hospital settings. Journal of advanced nursing, 72(12), pp.2980-3000.
Jenkins, M.G., Ford, J.B., Todd, A.L., Forsyth, R., Morris, J.M. and Roberts, C.L., 2015. Women׳ s views about maternity care: How do women conceptualise the process of continuity?. Midwifery, 31(1), pp.25-30.
Jouin, M., Gouriveau, R., Hissel, D., Péra, M.C. and Zerhouni, N., 2016. Degradations analysis and aging modeling for health assessment and prognostics of PEMFC. Reliability Engineering & System Safety, 148, pp.78-95.
Jutkowitz, E., Brasure, M., Fuchs, E., Shippee, T., Kane, R.A., Fink, H.A., Butler, M., Sylvanus, T. and Kane, R.L., 2016. Care‐delivery interventions to manage agitation and aggression in dementia nursing home and assisted living residents: a systematic review and meta‐analysis. Journal of the American Geriatrics Society, 64(3), pp.477-488.
Kim, M.O., Coiera, E. and Magrabi, F., 2017. Problems with health information technology and their effects on care delivery and patient outcomes: a systematic review. Journal of the American Medical Informatics Association, 24(2), pp.246-250.
Moaddab, A., McCullough, L.B., Chervenak, F.A., Fox, K.A., Aagaard, K.M., Salmanian, B., Raine, S.P. and Shamshirsaz, A.A., 2015. Health care justice and its implications for current policy of a mandatory waiting period for elective tubal sterilization. American journal of obstetrics and gynecology, 212(6), pp.736-739.
Repo, J.P., Rosqvist, E., Lauritsalo, S. and Paloneva, J., 2019. Translatability and validation of non-technical skills scale for trauma (T-NOTECHS) for assessing simulated multi-professional trauma team resuscitations. BMC medical education, 19(1), p.40.
Weled, B.J., Adzhigirey, L.A., Hodgman, T.M., Brilli, R.J., Spevetz, A., Kline, A.M., Montgomery, V.L., Puri, N., Tisherman, S.A., Vespa, P.M. and Pronovost, P.J., 2015. Critical Care Delivery: The Importance of Process of Care and ICU Structure to Improved Outcomes An Update From the American College of Critical Care Medicine Task Force on Models of Critical Care. Critical care medicine, 43(7), pp.1520-1525.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



