Enhancing Person-Centred Care Approaches
Part 1:
Introduction
According to NHS, person-centred care is the approach in which specific focus on the patient is created to ensure promoting their autonomy and independence, deliver choice of making care decision and controlling high-quality care support. In this approach, the patients are regarded as equal partners by the nurses to plan, develop and assess care to meet their needs in an appropriate manner (NS England, 2018). In this study, reflective account of person-centred care is to be presented for which the holistic approach to person-centred care is to be discussed. The review of personal practice regarding person-centred care in different support settings is to be explained. Moreover, ways to improve personal behaviour and skills in service support provision is also to be planned and discussed.
P1 Comparing the way medical and social model is related to person-centred care
The Medical Model considers the human body to have complex mechanism of system and advocates treatment of the symptoms with the use of medical procedures and interventions (Fuller, 2017). Thus, medical model in regard to person-centred care mentions that the health professionals are to specially diagnose health of each of the patients to determine which key symptoms of disease are faced by the individual patients. The health professionals are then required to provide specific medical intervention for each of the patient unique to their health condition, symptoms and diagnosis by making shared decision to ensure achievement of person-centred care. The Medical Model of Health also considers providing treatment by taking into account the social environment in which the patient lives and complementary system (McSherry, 2016). In this context, the medical model mentions that to provide person-centred care individuals social and physical environment of the patients are to be assessed and determined. This is to understand the nature of care best suited and specific for the patients as per their living condition to ensure their well-being. In contrast to Medical Model, the Social Model of Health consider social, economic and cultural factors that influence health and social care to develop understanding of the way stressors are to be managed for preventing diseases. This model mainly focuses on developing healthcare policies, awareness and education to ensure enhanced health of the patients (Ostaszkiewiczet al. 2018). Thus, social model in regard to person-centred care mentions the healthcare professionals to determine the specific healthcare policies and systems to be used to deliver person-centred care to the patients in meeting their personal care needs and demands. Moreover, the model mentions to assess the health awareness and education regarding illness among specific patients so that in person-centred care the health professionals can accordingly provide information regarding controlling their health to the patient. This is to ensure patients have ability to make informed decision and better understand of controlling and preventing diseases along with meeting their specific needs.

The only similarity existing between the social and medical model for person-centred care is that they both intend to promote enhanced health and well-being of the individual through person-centred care in the end (Sedler, 2016). This is because social model by improving specific social, economic and environmental situation compared to medical model that intends to use specific medication are trying to enhance health of the patients in person-centred care. Thus, both the model are required to work alongside to ensure enhanced care is provided to meet holistic needs of service users.
P2 Discussing the way to adopt a person-centred care approach
During planning and implementing healthcare program for individuals, the person-centred care approach can be adopted through development of effective communication with the patients in a safe environment. This is because effective interaction with the patients in safe condition leads them to reveal their care needs and demands to the health professionals without fear of losing privacy or confidentiality. It leads the health professionals accordingly determine the person-specific care to be delivered to each of the patients and they accordingly plan the care program for them to offer the patient quality care satisfaction (Sjögrenet al. 2017).As argued byEideet al. (2017), lack of communication leads to hindered person-centred as the basis of shared decision making in care planning could not be reached. This is because without interaction holistic information of probable care allowed to be used by the patients could not be mentioned by the health professionals. It leads the patients unable to develop informed consent and make share decision that are key aspects of person-centred care (Sundleret al. 2020). Thus, communication with patients is required for adopting patient-centred care in developing individual healthcare program for patients so that the healthcare professionals allow patients to make shared decision with them in planning care. In planning healthcare program for individuals, the person-centred care can be adopted by providing equal opportunity towards involvement in care for all patients and by showing them respect along with dignity. This is because equal opportunity would avoid discrimination of patients from informing their choice of care and respect along with dignity would make patients trust the healthcare professionals in developing shared care decision to support framing an effective person-centred care plan (Donnelly and MacEntee, 2016). The person-centred care approach in framing healthcare program can be adopted by the health professionals by empowering the service users to inform their care and availing feedback from them. This is because it would make the service users or patients develop ability to be architect of their care plan and mention health professionals to create changes in person-centred care plan according to update care needs of the patients to ensure their delivering specific acre (Cotter et al. 2020).
M1 Reviewing the challenges with application of person-centred care in the own workplace
In the current settings, the challenge with application of person-centred care includes staffing constraints and lower level experience of the staffs to deliver the approach. This is because person-centred care requires increased number of healthcare staffs to individually deliver and communicate specific care to the patients which when not available create workload on the existing staffs. However, it could be resolved with recruitment of adequate nursing staffs so that the workload is shared and nurse-to-patient ratio is improved which would allow nurses to specially provide care to each patient allowing establishment of person-centred care (Ashwoodet al. 2018). Moreover, the healthcare staffs require specific knowledge about communicating information regarding health intervention in person-centred care to make the patients develop informed consent and shared decision in planning their care (Peate, 2016). Thus, lack of availability of the knowledge among the staffs in current settings creates hindrance for them to successfully provide person-centred care. In order to develop effective communication by the nurses with patients to deliver person-centred care, they are to be involved in training for communication. This is because it would lead them to identify the jargons to be used and way effective verbal and non-verbal communication is to be used in establishing successful conversation with patients (Machielset al. 2017). The presence of confidentiality and compassion is key toward developing person-centred care approach. This is because confidentiality and compassion allow patients to trust health professionals out of showcasing of their sympathy and support towards the patient’s health condition, in turn, making the patients comply with professionals in sharing their needs of care to be fulfilled individually (Moore et al. 2017). However, in the current setting, it is seen that nurses are unable to maintain the confidentiality of the patients along with do not follow effective healthcare principles to show valued and compassionate care to the patients. This has led the service users to show non-compliance in acting with the health professionals to help them institutionalise person-centred care approach. The issue is to be resolved by training the nurses regarding the way to maintain confidentiality and implementing strict actions against nurses who avoid providing care by following nursing care principles. This is because fear of punishment would lead nurses to be alert in delivering appropriate care by following nursing principles that mention compassion and confidentiality for the patients to be established (Hawkleyet al. 2018).
D1 Evaluating the way dilemma influence consistency in delivering person-centred care
In the current settings, the dilemma faced in delivering consistent person-centred care is rights and responsibilities of service users versus healthcare professionals. This is because the care expressed to be needed by the service user at times in person-centred care approach is considered to be inappropriate in ensuring them have enhanced care (Walker and Deacon, 2016). However, the health professionals in respecting the rights of the service users are unable to avoid delivering the care. In addition, they also have the right to ensure high-quality care been provided to the patients under their supervision in person-centred care approach (McCance and McCormack, 2017). Thus, it leads to develop dilemma among the healthcare professionals whether to abide by their right of deciding care for the patients or follow the demanded care which may not be useful for the patient to enhance their health in the person-centred care approach.This, in turn, creates inconsistency in delivering person-centred care to the patients in effective manner out of inability to decide whose rights is to be supported. In some cases, it is seen that the healthcare professional misuse their rights and responsibilities by decide wrong care for the patient out of negligence (Kadookaet al. 2017). In this condition, the dilemma acts to ensure better care to the service users as the services chosen by them are appropriate and error free for their health thus acing as strength to ensure consistent person-centred care is provided to patients.The other dilemma that influences consistency in delivering person-centred care is abiding by the preference of service users versus abiding by the preference of care by healthcare professionals. This is because preference of care varies among individuals and service users being unable to understand effective impact of certain treatment may prefer to avoid approving to choose the intervention which could be more effective for their health. Since professionals according to NMC are to abide by choice of patients in person-centred care, they develop dilemma whether to follow the care asked for or deliver care which is actually effective for the patient (NMC, 2018).In some cases, it is seen that for the profit of the organisation, the healthcare professional tries to provide costly care which are not preferred by the patients (Fogliaet al. 2019). In this situation, the dilemma of providing care as per service user preference and healthcare professional preference acts as strength because abiding by the NMC, health professionals are made to provide preferred care made by the patients. This helps the patient avoid increased financial cost of care that was intended to be caused by the health professional for healthcare organisation’s profit.
P5 Producing a comparative reflective account of own person-centred care provision in different workplace settings
In present, the reflective account for person-centred care in different workplace settings, the Rolfe's reflective model is to be used. The Rolfe's reflective model is to be used as it provided a simple yet systematic framework for self-reflection to understand personal strength and weakness along with the way limited skills are to be improved (Scates and Dening, 2018). The three stages of Rolfe’s model are What?, So what? and Now What?.
1st experience:
What?
In the dialysis unit, while offering person-centred care I ensured effective mentoring of the patients are done to make them have skills and knowledge of creating valuable decision regarding their care needs to be fulfilled. However, I was unaware of the actions to be taken during mentoring of patients so that their care decision does not become inappropriate for their health.
So What?
The mentoring of the patients to determine their own care needs was an essential act. This is because being a nurse it would help enhanced care to be planned with engagement of patients that ensures providing the patient appropriate and satisfactory healthcare support during dialysis (Bowling et al. 2016). However, the lack of action to ensure effective mentoring where the patients demand inappropriate care led to create dilemma for me as a nurse to deliver quality care.
Now What?
I require mentoring patients to make them take informed decision in such a way so that did not make inappropriate demands of care. This is to be established by me by providing effective evidence to the patients and being a nurse personally support them in taking collaborative care decision with me.
2nd experience:
What?
While working in the diabetic ward, to deliver person-centred care, I ensured that expectations and needs of each patient are adequately analysed to determine the differences in care demands made by each of them in controlling their blood sugar level. However, in the diabetic ward, I failed to keep effective account of different specified medication provided to each patient during delivery of person-centred care.
So What?
The action in the diabetic ward led to develop provision for me as a nurse to deliver individualised person-specific care that is centred on different and similar needs of the diabetic patients to be fulfilled. However, inability to track individual medication needs of patients in diabetic ward during person-centred care led me to execute medication error which created deteriorated health impact on the patients to some extent.
Now What?
The experience led me to understand I require improving my ability to determine different medication to be provided to patients suffering from same health condition. This is to be executed by accessing training in medication management and administration to the patient along with developing increased awareness in differentiating similar medication for patients with similar health condition.
Comparison of the reflective account
What?
The comparison of the two reflective account mentions that I had effective understanding of rules and NMC Code of Practice to be followed in both the experiences. This is because NMC Code of Practice mentions that informed consent of patients regarding care are to be accessed and care is to be provided in best interest (NMC, 2018). In second the experienced, I expressed effective skill to abide by care in best interest of the patient and in first experience, I tried accessing informed consent from patients as mentioned in NMC Code of Practice. However, it is seen that I lack effective mentoring ability of the patients in allowing them take care decision in the first experience whereas I lacked medication management ability in the second experience.
So What?
The abiding with the NMC Code of Practice helps the nurses avoid any legal issues towards them (NMC, 2018). Thus, abiding with the care principles in both experiences I as the nurse was able to avoid creating ay legal issues while care delivery. As argued by Jemberet al. (2018) medication error leads nurses to deteriorate health of the patients. Thus, the medication mismanagement was a problematic skill for me. Moreover, hindered mentoring of patients to deliver inappropriate informed consent results nurse’s experience deteriorated health support to be provided to service users.
Now What?
On comparing the two experiences, I understood that training to mentor patients in making appropriate care decision is to be accessed by me. Moreover, I felt that I require to consult pharmaceutical agents in identifying how similar medication for similar patents are to be kept separate to avoid medication error.
M3 Examining own effectiveness of managing own workload in a team in delivering person-centred care
The effectiveness of managing personal workload in a team while offering person-centred care is that it allows abiding by bonafide professional code of conduct and avoid creating unnecessary work pressure on others in the team (Donnelly and MacEntee, 2016). This, in turn, leads to deliver enhanced care to individual patients without unnecessary delay. As mentioned by Rosengren (2016), prioritising own work ensures delivery of care that is of utmost importance at the initial stage followed by less important services and allows understanding way work effort is to be managed. This ensures creation of a systematic workflow without delay, in turn, avoiding development of burden on others to help in a team to deliver enhanced person-centred support to the patients. Thus, prioritising workflow which is done in the current settings is effective in managing own workload in a team in the person-centred care as it avoided creating delay in work or extra burden on others to assist in performing duty of care. The development of effective communication between peers is required to be maintained by me to manage workload in a team while offering person-centred care. This is because it allows duties to be shared and innovative ideas to be interacted among staffs for implication in providing enhanced and quicker person-centred care to all patients. It ensures avoiding delay or accumulation of work that are created out of hindered problem-solving condition and lack of ideas for resolving issues at work by the healthcare staffs in person-centred care (van der Cingel et al. 2016). In the current person-centred care setting, effective communication between staffs in the team caring for the patients is established by me which is beneficial as it allowed me to sharing roles and responsibilities of care. This led to enhanced management of personal workload in them team as sharing ideas and roles help to cope with adversities that may create hindrance in accomplishing the target at work. As argued by Anker‐Hansen et al (2018), lack of flexibility and adaptability would hinder healthcare staffs to effectively manage workload in a team while offering person-centred care. This is because the care needs of the patients would be continuously changing and without adapting to their needs to delivery care would make healthcare staffs accumulate wide care services to remain unoffered. It makes them unable to ensure effective workflow to reduce burden of duties in a team. In the current person-centred care settings, adequate adaptability and flexibility at work are shown by me asa nurse which has createdeffective impact on managing workload as it allowed personal duties at work to be adequately fulfilled without being accumulated.
D3 Critically evaluating own and other’s practice to allow consistent quality care in different healthcare settings
In mental healthcare settings, own practice implemented to ensure consistent delivery of high-quality person-centred care includes supporting or mentoring others in delivering care along with identifying areas of improvement in care. These are effective steps because mentoring or supporting other staffs in healthcare assist to resolve problems that hinders delivery of care. Moreover, determination of areas of improvement helps to identify the care delivery aspects to be changed to ensure unnecessary delay in consistent offering of support to patients (Ballard et al. 2018). However, others in the team of delivering person-centred care in the settings focussed on resolving conflict between team members to ensure consistent and high-quality care delivery. This is an effective approach because conflict resolution between team members helps them to work in collaborative manner with enhanced trust towards one another. It leads to make them feel valued and support each other in ensuring consistent care delivery of care to be made towards the patients (Maassenet al. 2017). The weakness faced by me while delivering person-centred care in the settings was that I lacked attention to detailed needs and demands of care of patients which led to create inconsistency in care. The lack of understanding of detailed needs and demands of care of patients leads the care unsuccessful to deliver holistic care which in turn negatively affects the patient. This is because some of their care needs remains unfulfilled which negatively affect the patient’s ability to attain effective well-being (Chong and Matchar, 2017). In case of others in the team delivering care, I found that they lack effective critical thinking skills. Thecritical thinking skills are essential for the nurses to resolve problem in care and create enhanced care support for patients (Sharpleset al. 2017). However, the others in the team of delivering person-centred care, failed to critically think to resolve conflicts in care decision with the patients resulting in hindered person-centred care to be delivered. In emergency care setting, own practice used for consistent delivery of quality care includes demonstration of appropriate leadership skills in directing work activities. This is an effective approach towards consistent care as effective leadership skills allow enhanced thinking and understanding of the way specific actions are to be taken to avoid any delay in care delivery and allows determining aspects to be implemented or changed in current care for its quality along with consistent delivery to patients (Brandstorpet al. 2016). However, the others in the team to ensure consistent delivery of quality care develop feedback from the patients regarding their care delivery. This is because feedback of care from patients allows healthcare workers to determine which aspects of care are good and which aspects are required to be changed or enhanced to ensure greater care satisfaction to the patients (Birnkrantet al. 2018). Thus, accessing feedback from patients regarding care was an appropriate technique performed by others in the settings to ensure delivery of consistent care as it allowed changes to be identified and made which otherwise would have created barriers to consistent delivery of care. The weakness faced by others in the emergency care was that they were unable to show compassion towards the patients. The compassion in care is essential to show value towards the patients and express support by understanding their pain regarding the health issue (Sinclairet al. 2018). However, the weakness faced by me in the emergency care was that I was unable to show cultural awareness. This is because I often tried to treat patients in the emergency wards without knowing from which culture they belong from and whether or not the care provided is supported in their custom that led me to face conflict in caring for the patients. This is because patients avoid to access care even if it is essential for them that are culturally supported in their society (Perez-Bret et al. 2016).
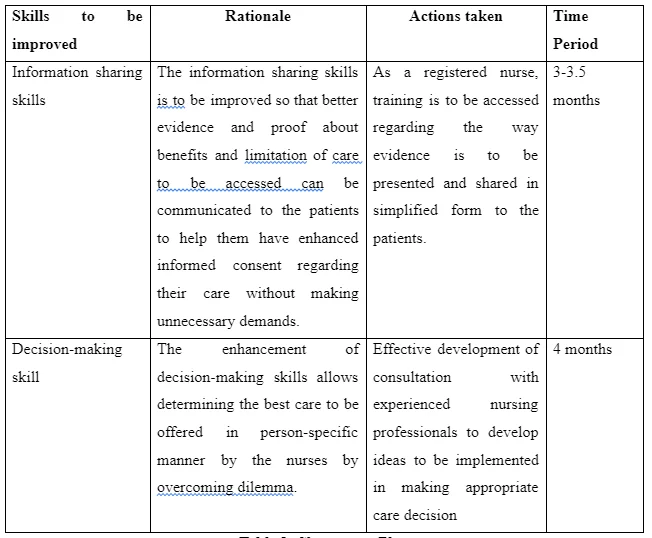
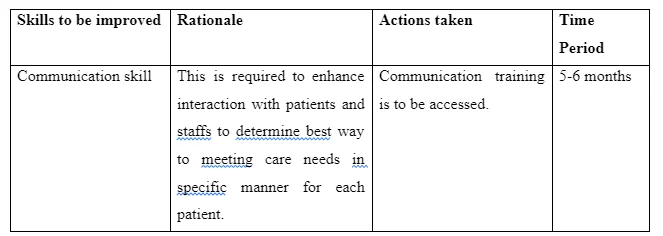
P6 Developing a short and long-term plan for improving person-centred care
The key skills identified to be present in nurses for delivering person-centred care include sharing of information, developing communication, involvement in decision-making, care coordination, offering respect and dignity to the patents and safe care planning. The Short-term plan for improving person-centred care is as follows:
The Medium-term plan for improving person-centred care is as follows:
The Long-term plan for improving person-centred care is as follows:
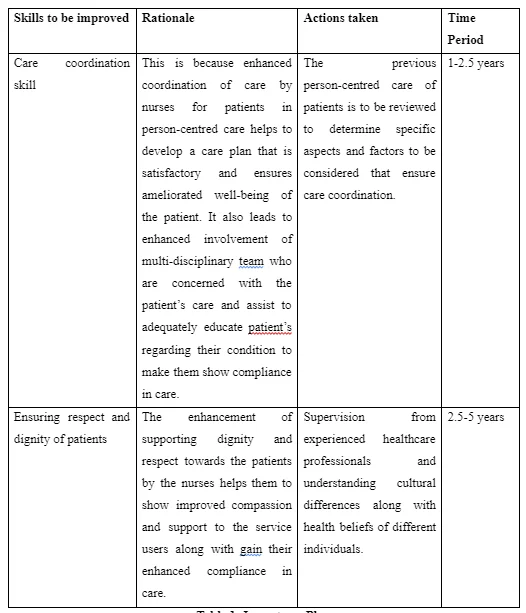
P7 Analysing practically the plans developed
The short-term and long-term plansare able to be practically implemented because in both cases training for upgradation of each of the skills identified is determined. As asserted by Surret al. (2016), undertaking training allows healthcare staffs to develop new skills and improve existing knowledge to deliver updated care. This is because training leads healthcare workers to learn tactics and information to overcome faults in existent skills along with specific actions to be enhanced as per new care developed to be delivered to the patients. Thus, use of training would contribute in collective effectiveness of the team at the workplace as continuous professional development can be ensured through its implementation. As argued by Mullan and Sullivan (2016), lack of consulting and identifying practical experiences of care from the supervisor leads healthcare workers unable to enhance their skills. This is because healthcare workers are unable to learn about the factors to be improved in the current delivery of care so that high-quality support can be created. In long-term plan, it is seen that supervision from the experienced health professionals to enhance the skill of respecting patients is to be done. This is a practical approach towards collective effectiveness for the team as the supervisor can inform by sharing their practical experiences about vital factors to be considered to show enhanced dignity and support to patients by the nurses which is principle of providing person-centred care.
M4 Implementing short-term plan in the workplace
In the first month, the short-term plan for improving information sharing skill is implemented. It is executed by initially attending training where ways in which appropriate sharing of information is informed. This is because using the learned techniques is going to help in overcoming obstacles faced with sharing information with the patients in turn supporting me as a nurse to help patients make effective informed decision-making for care with the shared data. I also planned to develop learning about the policies and regulation present in the organisation to be followed for sharing information such as use of simple terms, proof of evidence in form of pictures and others. The implementation of the actions led me to discover that I was able to deliver better information regarding care intervention needed by the patients. This is evident as the individuals indicated to show easier and enhanced understanding of the benefits and limitations of different care available to be accessed by them. The patients compared to previous implication of the plan were currently seen to be more interactive with me and expressed wish to avail further evidence if available regarding their care to make them develop effective informed consent and present shared decision regarding their care. The clarified delivering and sharing of information regarding care in person-centred care through pictures and evident content leads patients to make enhanced care decision regarding their care. This led to develop adequate and well-structured care plan that includes all the effective medical intervention for the patients as wished which offers them limited side-effects to be faced compared to other suggested intervention. The enhanced decision-making skills implementation in the workplace led me as the nurses avoid certain unintentional harm to the patients. This is because improved decision-making led me to understand in proactive manner the way determined healthcare practices could have affects the patients.
M5 Monitoring personal implementation of the plan
The monitoring of plan is done by performing clinical audits and accessing feedback from patients. This is because clinical audit helps to create a quality improvement in delivery of patient care by allowing systematic review of existing care being delivered (Grealishet al. 2019). Moreover, accessing feedback from patients regarding care helps the healthcare workers determine if their personal implementation of improvement plan is successful or not as enhanced care support experience of patient would indicate positive impact and vice-versa (Jakobssonet al. 2020). In relation to monitoring the currently implemented plan, through clinical auditing and feedback from patients, it is seen that information shared are well-understood than before by the patients. However, they reported to lack of adequate communication establishment regarding the information to resolve their doubts by the healthcare workers. Thus, it is suggested improved communication training is required to be availed by the nurses so that they can determine the way to further interact with patients in resolving their doubts after successful sharing of information regarding their care.It is also seen by analysing the feedback that better care decision for the patients are being taken than before by the nurses. This is evident as patients reported less error in care to be faced and informed most of their needs are being effectively fulfilled which were previously not done in the same way. The clinical audit mentioned that better care coordination is reached for patients as nursing staffs are seen to more intricately share information and work with one other than before to deliver care. The nurses are also seen to work in collaboration with multi-disciplinary team after the implementation of the play in collaboratively coordinating care to the patients.
D4 Critical reflective action plan
In order to enhance personal and professional development in delivering person-centred care by me, I intended to undertake critical reflection of my duty of care and pay attention to specific details while delivering care. This is because critical reflection of care duties and paying attention to care details allows nurses and healthcare workers to develop in-depth learning of their experiences enhance care quality (Xiao and Zhu, 2019). As argued by Park et al. (2018), for enhanced professional development the healthcare professionals are to be well-knowledgeable about the professional codes and policies to be abided. This is because it allows them to determine the principles and values of care to be considered in future for better delivery of person-centred care to the patients by maintaining professionalism. Thus, I plan to increase my knowledge regarding more care policies and legislation to be abided in delivering better professional care. This is to ensure I have effective understanding of codes and values to be abided by in my profession to deliver person-centred care with professionalism In order to fulfil this, I am going to explore NMC Code of Conduct, Care Act 2014, Health and Social Care Act 2012 and other regulations and policies that inform professional codes in care intervention to be maintained for person-centred care. The development of effective cultural awareness is required by the nurses in person to deliver culturally-approved care to the patients (Kaihlanenet al. 2019). The cultural awareness improvement is to be done for persona; development so that I am able to personally deliver respectful care to all patients of different cultures. Thus, to support further personal development separate training for understanding different cultural aspects of patients is to be taken by me. This is to ensure I have enhanced awareness of different culture and the customs of care present in each of them to be abided by me in delivering culturally aware care to any patients of any cultural background.
Conclusion
The above discussion informs that according to medical model while providing person-centred care the healthcare staffs are required to determine the care needs of the patients based on their health efficiency and deliver care intervention that are medically approved. The person-centred can be adopted by showing respect to patients, providing safe environment of care, communicating with patients, availing informed consent and others. The comparative reflection of person-centred care indicated that in different settings various aspects and factors are considered such as mentoring of patients, determining expectation of patients and others. The short-term plan for improving person-centred care includes enhancement of information sharing and decision-making skill of healthcare professionals. The long-term plan to improve person-centred care includes enhancement of respect and dignity showing skill, communication and care coordination skill.
Part 2:
Introduction
Person-centred care provides support individuals and healthcare workers develop skill and knowledge along with confidence in delivering quality support to the service users (Santana et al. 2018). In this assignment, the policies, legislation and regulations required for effective person-centred care for John are to be discussed.
P3 Discussing the aspects of different legislation for person-centred care
The Care Act 2014 informs that it is the duty of the local council to promote well-being along with independence of the working-age disabled adults and elderly to ensure their well-being (legislation.gov.uk, 2014). In person-centred care provision for John, the use of the Act is reflected. This is evident as according to the suggested guidance in the Act intervention of the local authorities are done for providing John’s preferred activities such as walking, playing video games and others. It is to enhance his health and well-being irrespective of his learning disability and challenging behaviour. The section 135 of Mental Health Act 1983 informs that a person can be removed from a dwelling if it is under consideration that the individual has a mental illness and required effective attention along with need of medical intervention (legislation.gov.uk, 1983). The Act is seen to be implemented in case of John where due to his challenging behaviour he is been removed from the housing and made to spent a long-time at the hospital to receive care for his health condition. The Health and Social Care (Safety and Quality) Act 2015 informs that reduction of harm to be suffered by patients and other service users for the care offered is to be made for ensuring their well-being (legislation.gov.uk, 2015). The Act is considered to be applied in case of John according which risk to be faced by the individuals is assessed and enhanced care plan is framed to ensure his adequate well-being. The section 117 of the Mental Health Act 1983 informs that aftercare services that are intended to meet the raised needs of the mentally ill people are to be provided. This is to ensure risk in reduction of worsening of the mental health condition for which the patient may have to go for readmission to the hospital (legislation.gov.uk, 1983). This Act is effectively used in framing person-centred care of John that is evident as analysing his past condition it is seen that John is required to remain involved in less social interaction for a stable health condition. Thus, the after services are accordingly arranged for John in which the local authorities ensured he has less interaction with people while going for walks and travels only with his support workers. This is to avoid him being into bigger crowd that is responsible for deteriorating his mental condition and readmission to hospital as seen in previous condition.
M2 Assessing challenges to interpret different legislation for planning person-centred care
In the Care Act 2014, to promote well-being the local authorities are required to understand and analyse the care needs of the patients along with share the information with others to arrange care (legislation.gov.uk, 2014). However, the challenge raised in this condition is maintaining confidentiality and privacy of the patients. This is because during care arrangement by the local council through discussion of care needs of the patients it may lead the information to be leaked in public due to unavoidable circumstances. It leads to expose identity of the individuals making them vulnerable to abuse or harm in the society (Gondeket al. 2017). For instance, while arranging care for John by the local authorities, there are chances of revelation of his hindered mental health condition which may raise panic among people for considering the person to be abusive. This would lead towards harming the individual by the common individuals in the society.The strength of managingconfidentiality and privacy of the patients which as currently acted as a challenge is that it makes the nurses ensure safety to the patients by avoiding to reveal their personal health information (Duffy and Kelly, 2017). For example, maintaining confidentiality and privacy of John's condition would lead him avoid to be considered as vulnerable individual in the society that would ensure him to be able to socially engage with others as they are no panic by his presence. The challenge to be faced in implementing Health and Social Care 2015 is that hindered identification and reduction of risk healthcare services may occur for the patient. This is because the health professionals or care providers may not have adequate knowledge regarding the way risk is to be identified and strategies to be used for lowering the intensity of risk (legislation.gov.uk, 2015). Thus, it may create problem for John to be unable to be protected from harmful situations to ensure his enhanced health. The strength of risk management in care is that it leads the nurses become aware of the specific condition in care are to be avoided for the patients so that any risky consequences can be avoided (Querstretet al. 2020). Thus, overcoming the challenge of risk management and identification in healthcare would lead John to avoid facing any further harm in the society. In implementing the Care Act 2014 and Mental Health 1983 for person-centred care of John, the challenge to be faced is delivering anti-discriminatory services and ensuring quality along with diversity. This is because the personal beliefs of the support workers regarding mental health patient may influence them to provide hindered and unequal care to manage their health that may create deteriorated health management of individuals like John (Sharp et al. 2016).The strength of anti-discriminative and quality care in mental health is that it allows showing value and respect towards patients and equal care for them to effectively enhance their health (Rothermundet al. 2017). In this context, anti-discriminative care would offer John the ability to get equal support like other patients suffering from different diseases in the society along with avoid showing him neglect for his mental condition, in turn, showing value and respect towards him.
Take a deeper dive into Enhancing Professional Growth in Healthcare with our additional resources.
P4 Suggesting solutions for problems to be encountered in implementing specific healthcare policies
The solution to resolve confidentiality and privacy issues in Care Act 2014in offering care to individuals like John includes use of secured password to protect the personal and health information of the individual. This is because securing personal information of patients through password during electronic health record storage helps to protect their information to remain private and accessible to only concerned individuals (Kuziemskyet al. 2018). In addition, to protect confidentiality of the patient while offering care under the Care Act 2014, it is to be ensured by the health professionals and social care workers that information regarding the patient is shared in a safe environment where only determined professionals required to be involved in care for John are present. This is because it would avoid the personal health information of patient like John to be passed in the public as a result of presence of inappropriate people who are not required to support his health (Ulinet al. 2016). According to NMC Code of Conduct, the nurses are required to avoid influence of their personal beliefs in arranging care for the patient. This is to ensure non-discriminative and equal care being provided to all (NMC, 2018). Thus, while implementing Care Act 2014 and Mental Health Act 1983, the nurses are to follow the NMC Code of Conduct to avoid challenges of including discriminatory care towards patients like John. The Whistleblowing is referred to informing concerned authorities regarding illegal practices within care environment to support enhanced well-being of the patients (Ash, 2016). Thus, Whistleblowing could be included as solution to resolve challenges with illegal working environment that do not support successful implementation of different care legislations. In order to resolve lack of adequate skill and knowledge challenges towards implementing Health and Social Care Act 2015, effective training for risk assessment to be delivered to the healthcare workers and professionals. This is because it would help them to have skills and knowledge regarding the way to identify risk in care and take actions to reduce them to ensure principles mentioned in the Act are appropriately followed (Bullenet al. 2019).

D2 Critically evaluating impact of health and safeguarding legislation at the workplace
In meeting legislative requirements of Care Act 2014, the presence of health and safety is for patients is essential as it leads the healthcare staffs aware about the way care actions are to be performed so that any unnecessary injuries and illness are avoided (Rossiteret al. 2020). This is evident as by understanding way health and safety for John is to be established through Care Act 2014, it would lead the support workers understand specific care practices to be offered to him so that he no more runs away from the current abode as done previously happens further. This in turn also meets the other legislative requirement of Care Act 2014 which indicates to offer quality care to the patients by the local authorities. In meeting legislative requirement, adequate healthcare staffs are required who would be responsible for offering person-centred care to patients. In order to ensure adequate staffs are available, the health and safety is effective as it leads to lower absence of healthcare staffs from the care environment, in turn, allowing adequate human resource to be present to deliver enhanced care a required by the patient. This is because health and safety lead the support workers feel valued at work out of the safe working environment where there is no risk for them to be harmed (Buckley et al. 2018). The effectiveness of Health and Social Care Act 2015 in healthcare is that it promotes improved productivity at work to be shown by the healthcare staff. This is out of their improved morale and value to get informed of the way safe working environment is to be maintained for patients with the help of the Act(Nilsson et al. 2019). As argued by McCance and McCormack (2017), lack of implication of health and safety legislation at the workplace leads to raise expenditure for the organisation. This is because damages caused due to safety issues by not following legislative action require increased finances. Moreover, lack of implementation of health and safety legislation such as Health and Social Care Act 2015 lead to turnover of healthcare staffs making the organisation spend increased amount of finances to recruit new staffs in managing effective implementation of legislation for care. Thus, to lower expenditure in managing the workplace and ensure effective environment that meet legislative requirement, the health and safety at workplace is required. In meeting legislative requirements, health and safety within healthcare at the workplace is essential as it is under the professional code of practice. This is evident as the NMC Code of practice informs health and safety in healthcare environment is to be assured so that safe working by healthcare staffs and secured care for the patient is ensured (Scales et al. 2017).
Conclusion
The above discussion informs that Care Act 2014, Mental Health Act 1983 and Health and Social Care Act 205 are key legislations used for managing care regarding John. The challenges to be faced while using the legislations to care for John include influence of personal beliefs, discrimination and others. The solutions involve providing training to healthcare professionals, supporting whistleblowing and others. In meeting legislative requirements, health and safety is required as it ensures retaining of healthcare staffs to deliver care, raise productivity at work, enhance care quality and others.
References
Anker‐Hansen, C., Skovdahl, K., McCormack, B. and Tønnessen, S., 2018. The third person in the room: The needs of care partners of older people in home care services—A systematic review from a person‐centred perspective. Journal of clinical nursing, 27(7-8), pp.e1309-e1326.
Ashwood, L., Macrae, A. and Marsden, P., 2018. Recruitment and retention in general practice nursing: What about pay?. Practice Nursing, 29(2), pp.83-87.
Ballard, C., Corbett, A., Orrell, M., Williams, G., Moniz-Cook, E., Romeo, R., Woods, B., Garrod, L., Testad, I., Woodward-Carlton, B. and Wenborn, J., 2018. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised controlled trial. PLoS medicine, 15(2).pp.78-90.
Birnkrant, D.J., Bushby, K., Bann, C.M., Apkon, S.D., Blackwell, A., Colvin, M.K., Cripe, L., Herron, A.R., Kennedy, A., Kinnett, K. and Naprawa, J., 2018. Diagnosis and management of Duchenne muscular dystrophy, part 3: primary care, emergency management, psychosocial care, and transitions of care across the lifespan. The Lancet Neurology, 17(5), pp.445-455.
Bowling, C.B., Plantinga, L., Hall, R.K., Mirk, A., Zhang, R. and Kutner, N., 2016. Association of nondisease-specific problems with mortality, long-term care, and functional impairment among older adults who require skilled nursing care after dialysis initiation. Clinical Journal of the American Society of Nephrology, 11(12), pp.2218-2224.
Brandstorp, H., Halvorsen, P.A., Sterud, B., Haugland, B. and Kirkengen, A.L., 2016. Primary care emergency team training in situ means learning in real context. Scandinavian journal of primary health care, 34(3), pp.295-303.
Donnelly, L. and MacEntee, M.I., 2016. Care perceptions among residents of LTC facilities purporting to offer person-centred care. Canadian Journal on Aging/La Revue canadienne du vieillissement, 35(2), pp.149-160.
Donnelly, L. and MacEntee, M.I., 2016. Care perceptions among residents of LTC facilities purporting to offer person-centred care. Canadian Journal on Aging/La Revue canadienne du vieillissement, 35(2), pp.149-160.
Fuller, J., 2017. The new medical model: a renewed challenge for biomedicine. CMAJ, 189(17), pp.E640-E641.
Grealish, L., Simpson, T., Soltau, D. and Edvardsson, D., 2019. Assessing and providing person-centred care of older people with cognitive impairment in acute settings: threats, variability, and challenges. Collegian, 26(1), pp.75-79.
Jakobsson, S., Ringström, G., Andersson, E., Eliasson, B., Johannsson, G., Simrén, M. and Jakobsson Ung, E., 2020. Patient safety before and after implementing person‐centred inpatient care—A quasi‐experimental study. Journal of clinical nursing, 29(3-4), pp.602-612.
Jember, A., Hailu, M., Messele, A., Demeke, T. and Hassen, M., 2018. Proportion of medication error reporting and associated factors among nurses: a cross sectional study. BMC nursing, 17(1), p.9.
Kadri, A., Rapaport, P., Livingston, G., Cooper, C., Robertson, S. and Higgs, P., 2018. Care workers, the unacknowledged persons in person-centred care: A secondary qualitative analysis of UK care home staff interviews. PloS one, 13(7).pp.34-56.
Kaihlanen, A.M., Hietapakka, L. and Heponiemi, T., 2019. Increasing cultural awareness: qualitative study of nurses’ perceptions about cultural competence training. BMC nursing, 18(1), pp.1-9.
Maassen, E.F., Schrevel, S.J., Dedding, C.W., Broerse, J.E. and Regeer, B.J., 2017. Comparing patients’ perspectives of “good care” in Dutch outpatient psychiatric services with academic perspectives of patient-centred care. Journal of Mental Health, 26(1), pp.84-94.
Machiels, M., Metzelthin, S.F., Hamers, J.P. and Zwakhalen, S.M., 2017. Interventions to improve communication between people with dementia and nursing staff during daily nursing care: a systematic review. International journal of nursing studies, 66, pp.37-46.
McCance, T. and McCormack, B., 2017. The person-centred practice framework. Person-centred practice in nursing and health care: theory and practice, 2, pp.36-64.
McSherry, W., 2016. Reintegrating spirituality and dignity in nursing and health care: A relational model of practice. Stories of Dignity within Healthcare: Research, Narratives and Theories. Edited by O. Tranvåg, O. Synnes and W. McSherry. Keswick: M&K Publishing, chp, 6, pp.75-96.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M. and Wolf, A., 2017. Barriers and facilitators to the implementation of person‐centred care in different healthcare contexts. Scandinavian journal of caring sciences, 31(4), pp.662-673.
Mullan, M.A. and Sullivan, K.A., 2016. Positive attitudes and person-centred care predict of sense of competence in dementia care staff. Aging & mental health, 20(4), pp.407-414.
Ostaszkiewicz, J., Dunning, T. and Streat, S., 2018. Models of care for aged care-social or biomedical?. Australian Nursing and Midwifery Journal, 25(7), p.45.
Park, H.Y., Hwang, M.S. and Kim, Y.H., 2018. Case-based learning through home care nursing specialists' critical reflection: application with patients using home mechanical ventilator. Journal of Korean Academic Society of Home Health Care Nursing, 25(3), pp.153-163.
Peate, I., 2016. Care Certificate Standards 5 and 6: working in a person-centred way; and communication. British Journal of Healthcare Assistants, 10(1), pp.36-43.
Sharples, J.M., Oxman, A.D., Mahtani, K.R., Chalmers, I., Oliver, S., Collins, K., Austvoll-Dahlgren, A. and Hoffmann, T., 2017. Critical thinking in healthcare and education. Bmj, 357.
Sinclair, S., Hack, T.F., Raffin-Bouchal, S., McClement, S., Stajduhar, K., Singh, P., Hagen, N.A., Sinnarajah, A. and Chochinov, H.M., 2018. What are healthcare providers’ understandings and experiences of compassion? The healthcare compassion model: a grounded theory study of healthcare providers in Canada. BMJ open, 8(3), p.e019701.
Sjögren, K., Lindkvist, M., Sandman, P.O., Zingmark, K. and Edvardsson, D., 2017. Organisational and environmental characteristics of residential aged care units providing highly person-centred care: a cross sectional study. BMC nursing, 16(1), p.44.
Surr, C.A., Smith, S.J., Crossland, J. and Robins, J., 2016. Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: A repeated measures study. International journal of nursing studies, 53, pp.144-151.
van der Cingel, M., Brandsma, L., van Dam, M., van Dorst, M., Verkaart, C. and van der Velde, C., 2016. Concepts of person-centred care: a framework analysis of five studies in daily care practices. International Practice Development Journal, 6(2), pp.1-17.
Walker, W. and Deacon, K., 2016. Nurses’ experiences of caring for the suddenly bereaved in adult acute and critical care settings, and the provision of person-centred care: A qualitative study. Intensive and critical care nursing, 33, pp.39-47.
Xiao, X. and Zhu, S.N., 2019. Critical reflection on the role of theater nurses in a multidisciplinary team for perioperative care in China. Frontiers of Nursing, 6(1), pp.27-33.
What Makes Us Unique
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



