Integrated Care and Staff Engagement in the Health Service
Introduction
The Health Service Executive (HSE) is a large and complex organisation which realises the importance of integrating care (Slaintecare 2017; HSE 2021) and staff engagement (MacLeod, 2009) to improve service quality and outcomes for staff and service users. A service user may have multiple appointments across several HSE teams both in acute and community services. Therefore the delivery of effective healthcare depends on effective collaboration and information across teams and services. According to Rosen et al. (2018, p.433), "the coordination and delivery of safe, high-quality care demand reliable teamwork and collaboration within, as well as across organisational, disciplinary, technical and cultural boundaries”. The implementation of integrated care may be determined by how effectively teams work together both within a service and across agencies. For those involved in researching similar topics, seeking healthcare dissertation help might provide valuable insights. Teams currently experience additional challenges with the increasing demands and constantly changing work practices and processes due to the COVID-19 pandemic. Leadership is fundamental to ensuring team success (Zaccaro et al. 2001) and sustaining the change required to deliver better service users and staff (Rosen et al. 2019).
This paper describes team working and discusses the processes which impact effective team working using the Input-Mediating-Process-Output model. The author also considers the benefits of team work to service users, staff and the organisation while also considering team leaders' role.

Real and Pseudo Teams
A team can be defined as a group of people who work on interdependent tasks (Salas 2015) and focus on achieving common goals (Overtveit, 1995) for which each member is mutually accountable (Katzenbach and Smith 2003). Managers tend to generously apply the label teams to groups due to the improved outcomes associated with team working (Lyubovnikova et al., 2015). However, a group of people has not deemed a team, and not all teams are effective (West and Lyubovnikova, 2013).
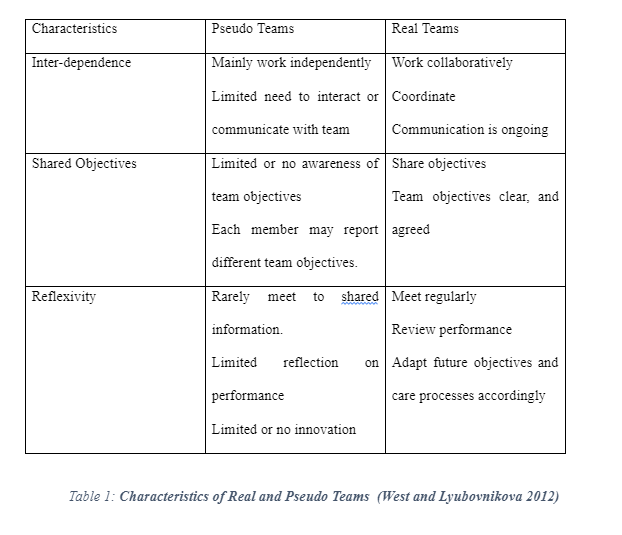
West and Lyubovnikova (2012) differentiate between pseudo and real teams using three characteristics; inter-dependence, shared objectives and reflexivity, as outlined in the table below.
Katzenbach and Smith (1993) demonstrated that the relationship between real teams improved team effectiveness and team performance in the graph below:

The Care Quality Commission (2010) conducted a study across the NHS and found that 90% of staff surveyed reported working in teams. Of this cohort, 40% were categorised as working in real teams while 50% worked in pseudo teams. Real team working is also associated with numerous benefits such as reduced errors, lower levels of patient mortality, reduced staff absenteeism and intentions to leave (Lyubovnikova et al. 2015). There is currently a dearth of literature regarding real and pseudo teams working in the HSE. Therefore, leaders working across HSE settings have to promote and audit real teamwork given the benefits to service users, staff and organisations.
Teams in the HSE
There are several types of teams throughout the HSE which can vary depending on the team’s purpose and structure (Ulrich and Crider, 2017). There has been a shift from co-located teams to virtual teams over the past year. There are many different theories to explore teams. Hollenbeck et al. (2012) propose teams can be characterised by three underlying components; skill differentiation, authority differentiation and temporal stability.
Skill differentiation
Traditional teams in healthcare were uni-disciplinary in nature i.e. a group of people with the same professional background working together to provide healthcare. Today there is a shift in the HSE towards multidisciplinary team (MDT) and interdisciplinary team working which is reflected throughout the policies guiding service delivery (HSE 2010, HSE 2020). A MDT is a group of people from different professional backgrounds working independently to organise and coordinate health care services to meet the service user’s goals and complex needs. An interdisciplinary team is a group of people from different disciplines working interdependently towards a shared goal. Children Disability Teams throughout Ireland are transitioning from MDT to the interdisciplinary team working. Research suggests that interdisciplinary teams reduce duplication of services, promote integrated healthcare, are more cost-effective, and are associated with increased staff and service user's satisfaction (White et al. 2013, O'Leary et al. 2012). An interdisciplinary team's success is strongly influenced by role clarity, high-quality communication and collaboration (Alotaibi et al. 2018). Leaders working towards an interdisciplinary team working should ensure structures are in place to facilitate the same.
Dig deeper into A Critical Appraisal of Person-Centred Approaches and Service with our selection of articles.
Authority differentiation
This describes the degree to which team members are involved in team decision making. Generally, teams with more significant authority differentiation have clear leadership or senior roles and can be bureaucratic (West & Lyubovnikova 2013). According to Nembhard et al. (2007), "shared decision making and respectful collaboration are vital to enabling improvement in health care". The HSE is striving towards collective leadership where staff are encouraged to engage in leadership roles and work together towards a shared purpose, inspiring innovation and creativity for better healthcare outcomes (HSE PNDC). Leaders are encouraged to adopt a lower authority differentiation to facilitate staff engagement in decision making. Core research (2020) recently studied staff's experiences during Covid-19 within the HSE. Staff reported increased involvement in decision-making; however, one out of five participants reported dissatisfaction with their managers' communication levels. Leaders need to consider engaging staff in communication and decision making by taking adequate time to listen and feel valued.
Temporal Stability
This refers to the lifecycle of a team which varies throughout the health service. Many teams maintain a somewhat stable composition over some time while other teams from and reform regularly. For example, Covid testing teams involve redeployed staff come together for a day of testing. They may not work together again depending on the Covid testing centres' demand and resources available. Teams with higher temporal stability levels experience more significant opportunities to develop effective team processes and interpersonal relationships (Lee et al. 2015). Given the current demands on healthcare services due to Covid-19, temporal stability is more than likely affected across the HSE. To ensure service efficiency and quality, leaders will promote policy, protocols, and standard operating procedures. One of Hollenbeck el al. (2015) model's disadvantages is that there are no objective measures of the gradients of skill differentiation, authority differentiation, and temporal stability. This may impact a leader’s ability to carry out high-quality research or audits.
Input-Mediating-Output-Process Model
Teamwork is important for quality and safe patient care. Interventions can improve teamwork but their influence relies on valid, reliable and practical measurement models (Abualrub, Gharaibeh, and Bashayreh 2012). The input-mediating-output-process model can augment current methodologies and improve access to real-time feedback on team interactions. Using this mode, large practical benefits to patients, care providers, and their colleagues can be realized by addressing the technical, cultural, theoretical, and methodological issues involved.

The model defines a team as consisting of two or more people who have specific roles and working together adaptively and interdependently toward shared goals (Rosen et al 2015). Teams can be collated or virtual (partially or wholly distributed in space). It also emphasizes on task work which refers to a clinical activity that does not demand interdependence. Such tasks can be completed with team member without input from other team members. This is particularly important because of balancing workload which requires that clinicians should complete their team tasks as well as individual tasks. In the model, teamwork is described as dynamic interactions among team members like communication and coordination events. The summation of teamwork and task work activities is what makes up team performance. In addition, the model describes team effectiveness as an assessment of the quality of team performance outcomes in relation to specified standards such as learning outcomes, team member satisfaction and viability, and task outcomes. There can also be multi-team systems which refer to networks of component teams sharing mutual goals that are interdependent with other teams.
This offers approaches to delineate strengths and weaknesses of the model through physical distribution of team members and specifying behavioral expectations for effective teamwork (Liu and Ulrich 2016). In healthcare, physical distribution of team members vary greatly, for instance, an intensive care unit with phases of collated-rounds-and distributed activity.
Teamwork can be measured using at least three categories of team outputs, namely, team learning, task efficiency, and affective outcomes. The measures can be sensor-based using alerts and alarms. Task efficiency is measured in terms of how fast clinicians react to alarms and alerts. Team learning can be assessed by evaluating changes in a priori defined patterns pf effective and ineffective teamwork or changes in communication structure (Herre 2010). Analyzing patterns of team interaction can provide insights into affective team outcomes like staff satisfaction.
The model captures a dynamic network of which clinician interacts with whom, and where, when, and how. It can contribute to interventions for improving team, individual, organizational, and unit learning in healthcare. For individual clinicians, the model can offer real time support for them to balance their individual workload efforts and give feedback on the quality and quantity of interactions with patients or other clinicians. For a team, the model can offer to augment traditional techniques of team improvement like self-guided team reflective activities such as identification of performance deficits. At the unit level learning, the model can serve to detect work system issues that can be addressed using procedures, policies, staffing, work processes, and equipment.
What contributes to the effective team and improve the quality of care
Effective communication among staff members positively impacts teamwork and encourages continuity and clarity with the patient care team (O’Daniel and Rosenstein, 2008). Communication, at its best, encourages collaboration, helps prevent errors, and fosters teamwork. With teams consisting of physicians, different nurses, and other healthcare experts, it is vital that they effectively and communicate with one another for building stronger work relationships, sharing resources, and solving problems. Effective communication enables team members to cooperate, exchange information, integrate and provide timely informed consent.
Decision making
Patient participation in decision-making is an essential aspect of effective patient care. They should be included because they might have vital information concerning their health which may help team members make effective decisions concerning the patients' condition (Labarrere et al., 2011). Patient participation also helps healthcare teams to make the right decision hence minimising decision errors.
Leadership
Leadership is an essential aspect of creating and sustaining the culture changes needed in adopting team improvement. Leaders should brief the members so that they can understand the goals, roles, and responsibilities, as well as the freedom to voice their issues (Katzenbach, and Smith, 2015). For instance, debriefing is a vital opportunity that enables teams to discuss their performances but only becomes effective under strong leadership. In hospital settings, the extent to which patient safety is prioritised is greatly affected by leadership (Ruchlin, Dubbs, Callahan 2004).
Role clarity
Shoddy team work is associated with role-boundary conflicts. Role conflicts among hospital staffs male them not able to assure patient safety and offer the required highest care standards (Kvarnstrom 2008). In addition, they cannot protect patients from all forms of harms that come from increasingly complex and powerful treatment.
Benefits of an effective team to staff and patient care
Rosen (2019) documents that quality derived from teamwork positively impacts staff members and organisational outcomes. Most research studies have linked the quality and safety of healthcare delivery to the quality of teamwork. Teamwork focuses on three main domains, which include: patient experiences, quality and safety of care, and clinical patient outcomes. For instance, as Wilson et al. (1995) documented, teamwork enhances communication and coordination of risks. In the same study, the authors found out that communication failure, which is an error of technical competence, was a likely cause of preventable patient deaths.
According to Lyubovnikova et al. (2015), effective teams create an engaging, positive and resilient workplace. Besides, the authors point out that hospitals with well-organised teamwork have lower rates of workplace illness and injuries, lower levels of staff intent to leave the organisation, and lower workplace violence and harassment experiences. Furthermore, the workplace climate due to team work correlates positively to the way staff engage and feel in their work leading to positive patient outcomes (Daugherty Biddson et al. 2015). Such a united workforce consists of staff members who are highly committed to and have a strong sense of ownership over their job responsibilities (Bwoers et al., 2011). Besides, teamwork quality is indirectly associated with the levels of burnt-out experiences by staff members. According to West et al. (2006), staff involved in events touching on patient safety are usually the second victims – in which hospital residents affected by medical errors have reduced quality of life, increased burnt-out, and depression.
Kusher and Date (2020) have established that inter-disciplinary rehabilitation team work coordinated through team conferences held weekly impacts patients suffering from a stroke. In a nutshell, the study indicates that useful inter-disciplinary team conferences during the rehabilitation of inpatients with acute stroke are essential in improving functional outcomes and managing long term costs. In this manner, effective team conferences assist in identifying patients at risk of developing medical complications and determining client-centred interventions. In their study, Dilworth, Philips and Rose (2011) concluded that hospital staff made fewer attributions of controlling very challenging behaviours to the patients when they worked in "an organisational service with a better quality." In another study by (Gomes and McVilly 2019 pg. 192), team functioning was observed to affect staff's perception, impact the willingness of staff to assist, and the subsequent quality of service delivery independent of individual staff attributes.

Conclusion
In modern healthcare settings, it is a rare phenomenon for patients to be under the only single provider's care. Instead, an interdisciplinary team of healthcare staff delivers patient care. In such a case, nurses ought to have the required skills and preparations to work as one team. Team processes and outcomes are significantly impacted by the organisational context, in which case organisational culture determines the team members' operating conditions. For instance, the norms of interaction in a hospital setup have been shown to promote effective team work. The Input-Mediating-Output-Process Model consists of pf inputs, mediators and outputs in the teams working collaboratively. It describes the way team processes can emerge from different environments and resources. The model establishes a better understanding of healthcare teams with patients. Effective communication, collaborative decision making, effective leadership, and role clarity contribute to an effective team and improve the quality of care. When teams coordinate care, they reduce stress levels that patients may experience and influence outcomes positively.
Additionally, teamwork reduces the number of issues associated with burnout in nurses. Nurses get support from other team members in making decisions since they are not the only care providers. In short, healthcare teams working together can achieve goals such as enhancing patient safety, improving clinical performance, raising efficiency and lowering healthcare costs, and cutting down on medical errors.
Continue your exploration of Navigating Roles and Responsibilities in Multidisciplinary Healthcare Teams with our related content.
Reference
AbuAlRub, R.F., Gharaibeh, H.F. and Bashayreh, A.E.I., 2012, January. The relationships between safety climate, teamwork, and intent to stay at work among Jordanian hospital nurses. In Nursing forum (Vol. 47, No. 1, pp. 65-75). Malden, USA: Blackwell Publishing Inc.
Buttigieg, S.C., West, M.A. and Dawson, J.F., 2011. Well-structured teams and the buffering of hospital employees from stress. Health Services Management Research, 24(4), pp.203-212.
Carter, A.J.W. and West, M., 1999. Sharing the burden-teamwork in health care settings.
Dawson, S., 2007. Interprofessional working: communication, collaboration..
perspiration!. International journal of palliative nursing, 13(10), pp.502-505.
Herre, C., 2010. Promoting team effectiveness: How leaders and learning processes influences team outcomes (Doctoral dissertation, Université de Fribourg).
Hill, A., 1998. Multiprofessional teamwork in-hospital palliative care teams. International Journal of Palliative Nursing, 4(5), pp.214-221.
Katzenbach, J.R. and Smith, D.K., 2015. The wisdom of teams: Creating the high-performance organisation. Harvard Business Review Press.
Labarre, C.A., Woods, J.R., Hardin, J.W., Campana, G.L., Ortiz, M.A., Jaeger, B.R., Reichart, B., Bonnin, J.M., Currin, A., Cosgrove, S. and Pitts, D.E., 2011. Early prediction of cardiac allograft vasculopathy and heart transplant failure. American Journal of Transplantation, 11(3), pp.528-535.
Liu, J. and Ulrich, C., 2016. Mediation analysis in nursing research: a methodological review. Contemporary nurse, 52(6), pp.643-656.
Lyubovnikovn, P.M., 2015. Real Team and Co-Acting Group Membership
MacLeod, D. and Clarke, N., 2011. Engaging for success: enhancing performance through employee engagement, a report to Government.
Mathieu, J., Maynard, M.T., Rapp, T. and Gilson, L., 2008. Team effectiveness 1997-2007: A review of recent advancements and a glimpse into the future. Journal of Management, 34(3), pp.410-476.
O’Daniel, M. and Rosenstein, A.H., 2008. Professional communication and team collaboration. Patient safety and quality: An evidence-based handbook for nurses.
O'Leary, K.J., Sehgal, N.L., Terrell, G., Williams, M.V. and High-Performance Teams and the Hospital of the Future Project Team, 2012. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. Journal of hospital medicine, 7(1), pp.48-54.
Rosen, M.A., Dietz, A.S., Yang, T., Priebe, C.E. and Pronovost, P.J., 2015. An integrative framework for sensor-based measurement of teamwork in healthcare. Journal of the American Medical Informatics Association, 22(1), pp.11-18.
Ulrich, B. and Crider, N.M., 2017. Using Teams to Improve and Performance. Nephrology Nursing Journal, 44(2).
West, M. (2003). Leadership clarity and team innovation in health care, The Leadership Quarterly, Vol. 14 No. 4-5, pp. 393-410.
West, M., Dawson, J., Admasachew, L. and Topakas, A., 2011. NHS staff management and health service quality: results from the NHS staff survey and related data. London: Department of Health.
White, M.J., Gutierrez, A., McLaughlin, C., Eziakonwa, C., Newman, L.S., White, M., Thayer, B., Davis, K., Williams, M. and Asselin, G., 2013. A pilot for understanding interdisciplinary teams in rehabilitation practice. Rehabilitation Nursing, 38(3), pp.142-152.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



