Integrating Physical and Mental Health
Introduction
The change proposal developed in the study has key aim to create increase in physical healthcare services for the patients in a psychiatric or mental rehabilitation unit. This is because physical and mental health are inter-related and avoiding one of their improvement would result to make the patients unable to regain proper well-being and sound health in life (Wickrama et al. 2020). The change suggested to be made will be introduction of physical healthcare unit at rehabilitation facility that will execute diet support, weight control management, smoking cessation activities and others. The patients will be referred to primary services based on the identification of their health concern such as people with hindered mobility are to be referred to physical exercise classes and others. Additionally, seeking healthcare dissertation help can provide valuable insights into best practices for implementing these changes. The patients admitted to the acute mental healthcare unit are referred to the rehabilitation unit as it assists them to overcome difficulties and impact of long-term and short-term mental health condition on physical health.
The change management will be organised in the rehabilitation ward that offers services and support to adults with mental health difficulties to be finally discharged to live a proper life in the community. However, during the 10th week of the placement, it was reported by the health professionals in the multi-disciplinary meeting organised that patients are facing challenges to access proper healthcare services to get effectively included in the society. This is evident as patients often require assistance from general practice and dentistry to get released in the wider society but they are facing difficulty in accessing those services and for making routine check-ups. Moreover, patients are found to be involved in less physical exercise and unhealthy diets which are making it unable for the health professionals to ensure them effective care to be rehabilitated into society. Thus, in making the change eight-step change management model developed by the NHS is to be followed. Further, the Plan, Do, Act & Study (PDSA) cycle is to be used to inform the way the change management is to be addressed.

Background
Individuals with serious mental illness (SMI) such as schizophrenia and bipolar disorder have a shortened life expectancy and a higher prevalence to physical health problems than the general population (Baxter et al., 2016). The side effects of hallucinatory medication, high smoking rates, inactive lifestyles, and impoverished diet - along with inequalities in healthcare provision - are all factors that may contribute to poor physical health (Cunningham et al., 2013). The UK National Institute for Health and Care Excellence (NICE,2018) guidelines for improving physical health for people with SMI state that primary care should monitor the physical health of people with psychosis. However, all to frequently, this does not happen in practice (Yeomans et al., 2014). In people with SMI, often their physical needs are overlooked as healthcare professionals more intricately focus on their mental health issues, in turn, neglecting or mistaking signs of physical illness to be the impact of psychiatric issues (De Hert et al., 2011).
In an attempt to improve the physical health of people with SMI, the English National Health Service (NHS) published the Five Year Forward View for Mental Health (2016) a report from the independent Mental Health Taskforce. The report states‘…by 2020/21, at least 280,000 people living with severe mental health problems should have their physical health needs met. They should be offered screening and secondary prevention reflecting their higher risk of poor physical health’. This will reduce the health inequalities gap’(NHS Five Year Forward Plan, 2016). Although the UK has primary and secondary care strategies for physical health screening and interventions, as set out in the aforementioned NICE guidelines(2018) and NHS Five Year Forward Plan (2016), there are no nationally agreed strategies for services to identify and manage physical health issues amongst service users with SMI (National audit of schizophrenia, 2014). In this respect, there are no established specialist interventions aimed at improving the physical health of people with SMI; instead, the same processes that are applied to the general population are used.
Continue your journey with our comprehensive guide to Mental Health Or Physical Health.
Implementing the change
Change Management Framework
The NHS Change Management Model to be used in the study is an 8-step approach in making sustainable and transformation change (england.nhs.uk, 2020). The NHS change management model is developed by experienced clinical professionals where structured and systematic information is provided regarding the way energy for change can be built across all phases of healthcare. Thus, the benefit of using the model is that it is reliable to make successful and sustainable change in healthcare industry to deliver improved healthcare (england.nhs.uk, 2020). In the study, the Lewin's change management model is not to be used as it provides a rationale and goal-oriented idea in making the change which though looks good theoretically but when implemented in the practical field may lead to create negative consequences. This is evident as the change developed in the model is not done by considering the feelings and experiences of the individuals who are to be involved in making the change (Bakari et al. 2017). In the NHS Change Management model, the change activities are done through shared purpose meaning all individuals making the change are considered in each phase to develop collaborative vision in successful accomplishment of the change (england.nhs.uk, 2020). However, in Kotter's Change Management Model, the limitation is that it is top-down model due to which co-creation of goals of change are not accomplished making many people involved in the change lack idea about the vision to be accomplished that may develop hindered change accomplishment. In addition, lack of shared purpose in all steps leads the people involved in the change show resentment and resistance to accept the change in using Kotter's model (Teixeira et al. 2017). Therefore, the model is not to be used in executing the change in the study.
In spread and adoption phase, the NHS change management model informs that idea of change is to be appropriately informed to all the people involved in making the change and they are required to accept the idea (england.nhs.uk, 2020). This indicates that nurses in the rehabilitation ward are to be informed for the need to change that is increase in delivery of physical healthcare services to the mentally-ill people. It is to be done by producing evidence to the healthcare workers in the ward regarding the way deteriorated physical healthcare is creating issues for the mentally-ill people to get effectively included in society. The use of leaflets and posters are required for spreading news regarding change in healthcare field as they act as visual and written modes to led healthcare workers understand the need and way changes are to be made to accomplish the vision communicated to them (Dunn, 2017). Thus, leaflets and posters should be displayed around the unit, detailing relevant information on the physical health clinic and related interventions. These should be written in easy-to-read and engaging format, to ensure service users can understand and are interested in the information.
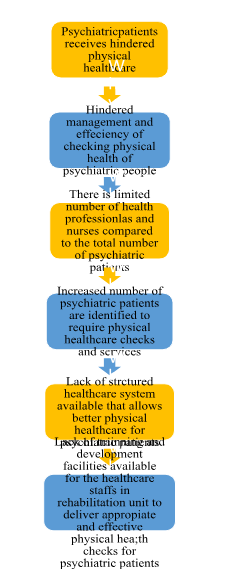
In regards to improvement tools, the 5 Whys Model is to be used in the study. The 5 Whys model leads to determine the cause-effect relationship of an identified problem for identifying the root cause that led to the rise of the issues (Augustsson et al. 2019). Thus, by using 5 Whys model, root cause of the current issues in delivering physical healthcare to mentally-ill people in the rehabilitation centre is be identified based on which actions are to be developed for making further change. The 5 why model explains the following:

In the project management phase, the NHS model informs that the intended change is to be planned, executed controlled and closed while working as a team to achieve the determined goals (england.nhs.uk, 2020). Thus, in the project management phase planning based on the identified root cause of the problem through 5 Whys model is to be done. The plan for making the change is to provide training to the existing staffs and increase number of staffs to deliver better physical health checks and services for the mentally ill people in the rehabilitation ward. In executing the plan, holistic involvement of the management and healthcare staffs in the rehabilitation ward is required who would take active approach in accomplishing the change. The controlling of the change determine would be done in the project management by continuously monitoring its progress in implementation and the closing of the project is to be done with successful implementation of the change.
In the measurement phase, the NHS informs to assess and monitor the progress and impact of the change. This is because measurement of performance of the change is able to determine whether or not the change-making actions implemented are effective to make the determined improvement (england.nhs.uk, 2020). Thus, the baseline measurement in this aspect would include examining mentally-ill patient’s present attendance in availing physical checks and services. The outcome measurement to be done involves assessing the percentage of patients compared to before the change are able to access effective physical healthcare in the rehabilitation ward to get effectively prepared in getting accepted in society.
The system divers in the NHS Change management model inform about the intrinsic and extrinsic motivators to be required in making the change. The intrinsic motivators are referred to personal motivating factors of the people involved in the change (Berdud et al. 2016). Thus, the staffs involved in making the change are to be ensured they develop a sense of belonging to make the change and develop sense of achievement by watching the accomplishment of the project. The extrinsic motivations are referred to the external factors which persuade the staffs in making the change to accomplish the goal (Bidee et al. 2017). In this aspect, the peer pressure, information regarding patient's satisfaction, availability of effective resources to make the change and development of effective teamwork are to be used as extrinsic motivation factors.
The motivate and mobilise part of the model is about engaging the stakeholders and ensuring that they are actively involved in the change project. It is important not to underestimate the significance of including all relevant stakeholders, in this case, staff; that is clinical and non-clinical staff. The latter is often the service users first point of contact with the setting. Motivating clinical frontline staff is essential to any quality improvement project, but it can be difficult as they are busy professionals. However, there are ways in which leaders can motivate and involve staff, for example:

In leadership by all, the NHS model informs to mention the nature of leadership style to be followed in accomplishing the improvement. In this change management, transformational leadership is to be used. The transformational leadership is the style where the leaders work along with the team for determining the change, developing vision for guiding the change through motivation and executing action in tandem with the staffs involved in making the change (Thomson et al. 2016). The transformation leadership is to be used in making this change because it would make the leaders work along with the staffs involved in creating the change to share innovative ideas and form effective plan for the change to be accomplished with minimum disruption in the daily operation of activities (Sligo et al. 2019). Therefore, transformational leadership would be effective for the leaders in the change to inspire the staffs in the rehabilitation ward to show proper participation and zeal in working with efficiency to deliver better physical healthcare opportunities for the mentally-ill patients to ensure their quality acceptance in the society. (Refer to Appendix 1)
Impact of the Change on Healthcare system
The proposed change is going to impact the healthcare system to improve screening, monitoring and management of physical health of the patients with SMI (severe mental illness). This is because introduction of physical healthcare facility within the mental rehabilitation unit would help to assess physical health condition of the mentally-ill patients. Moreover, it would lead to determine the nature of primary physical care required by the individuals, in turn, acting to improve their physical health which would also have positive effect on their mental health. It is evident as good physical health condition are seen to lower stress, depression, anxiety and other mental health symptoms in patients. In addition, better physical health leads mentally-ill people to develop effective physical efficiency in taking their care and better respond to mental treatment to show quicker progress to be effectively included in the society (Young et al. 2017). Thus, the change is going to impact on SMI patients to overcome physical health issues such as substance abuse, low body weight, physical ailments and others that are secondary effects of their mental illness.
Evaluation of the Change
The change evaluation is essential as it helps to determine to what extent the proposed change is successful and the further alterations require to ensure its better success. In order to evaluate the proposed change, feedback from the SMI patients in the rehabilitation ward is to be gathered. This is because effective feedback from patients helps to collect information about their reactions regarding the services provided to them (Bovendeerd et al. 2019). This indicates that the proposed change can be determined successful if increased number of patients with SMI in the rehabilitation unit providesfeedback that their physical health issues are properly screened and managed to ensure better health condition. The monitoring of healthcare system in the rehabilitation ward is to be done to determine the success of the proposed change. This is because through monitoring the amount of change and efficiency in executing physical screening and management of the patients can be identified among the healthcare staffs to evaluate extent of success of the proposed change.The interview of the patients is to be organised to evaluate the success of the change. This is because interview helps to gather emotions and feelings of the participants as well as their opinion regarding any change (Morain et al. 2017). Thus, by interviewing the patients it can de be determined to what extent they are satisfied with receiving the current physical healthcare screening and primary care services, in turn, helping to determine success of the change. This is because without improved patient satisfaction through the implemented change it cannot be determined to be successful.
Evaluating ways the proposed change would improve care quality
The change which is proposed is going to enhance the care quality by creating better physical health condition of the patients with SMI which going to ensure them improved and quicker inclusion in the wider society from the rehabilitation ward. This is because the patients will be able to achieve effective physical health screening and its management through referral to require primary healthcare services to ensure their well-being. Moreover, the proposed change would enhance physical ability of patients with SMI to take their own care, in turn, avoid being burden of care on others in the society.
Ways to inform the change
The change proposed is to be informed to the healthcare staffs and patients through audio and visual mode, written content and others. The audio and visual mode of communication is to be used for informing any change as visual images are seen to be better interpreted and remembered by the brain along with audio helps the viewers understand the content being shown to them (Mishkind et al. 2018). Thus, audio and visual communication are to be used for healthcare workers in the rehabilitation ward to understand the ay they are to manage their services to ensure proper physical screening and health management of the patients with SMI are done. The written communication helps to provide detailed information regarding any change in step-by-step process and assist it to be kept personally by the healthcare staffs to refer the information in changing their services (McLaughlin et al. 2017Thus, written communication is to be used for the patients and healthcare staffs in the rehabilitation ward to report roles and responsibilities to be performed by each of them so that effective physical health assessment of the patients is accomplished that is the intention of the proposed change.

Conclusion
Individuals with SMI have a shortened life expectancy and a higher incidence of physical health issues, relative to the general population. Although public health policies and clinical recommendations promote and seek to prioritise the physical health of these populations, they have been somewhat constrained in the approach to implementing interventions to support them. Introducing improvements in the way in which the physical wellbeing of people with SMI are supported in a rehabilitation setting can educate and signpost preventive services and promotes similar interventions across a greater range of settings. In this process, the NHS change management model is being used which informed that use of evidence of requirement of change is to be made for spread and adoption of the change, 5 whys and PDSA cycle is to be used as improvement tools, transformation leadership is to be used as leadership style and others to make the proposed change. The feedback and interview of patients along with health monitoring is to be done for determining the success of the change.
The iteration of the change is going to ensure better physical health management among the patients with SMI making the get effectively and more quickly get accepted in the wider society. This in turn is going to help the patients with SMI to experienced well-being and improved health. For instance, physical screening of patients with SMI having substance abuse and offering them according cessation services would improve their addiction issues. This in turn is going to help them have improved physical health as well as ability to manage self-care for resolving associated SMI assisting them to get properly included in the society.
Dig deeper into Integration of Telepsychology during the COVID-19 Crisis in Australia with our selection of articles.
References
Augustsson, H., Churruca, K. and Braithwaite, J., (2019). Mapping the use of soft systems methodology for change management in healthcare: a scoping review protocol. BMJ open, 9(4), p.e026028.
Bakari, H., Hunjra, A.I. and Niazi, G.S.K., (2017). How does authentic leadership influence planned organizational change? The role of employees’ perceptions: Integration of theory of planned behavior and Lewin's three step model. Journal of Change Management, 17(2), pp.155-187.
Baxter, A., Harris, M., Khatib, Y., Brugha, T., Bien, H., and Bhui, K. (2016). Reducing excess mortality due to chronic disease in people with severe mental illness: Meta-review of health interventions. British Journal of Psychiatry,208(4), pp. 322-329.
Berdud, M., Cabasés, J.M. and Nieto, J., (2016). Incentives and intrinsic motivation in healthcare. Gaceta sanitaria, 30, pp.408-414.
Bidee, J., Vantilborgh, T., Pepermans, R., Willems, J., Jegers, M. and Hofmans, J., (2017). Daily motivation of volunteers in healthcare organizations: Relating team inclusion and intrinsic motivation using self-determination theory. European Journal of Work and Organizational Psychology, 26(3), pp.325-336.
Boamah, S.A., Laschinger, H.K.S., Wong, C. and Clarke, S., (2018). Effect of transformational leadership on job satisfaction and patient safety outcomes. Nursing outlook, 66(2), pp.180-189.
Bovendeerd, B., De Jong, K., Colijn, S., De Groot, E., Hafkenscheid, A., Moerbeek, M. and De Keijser, J., (2019). Systematic client feedback to brief therapy in basic mental healthcare: study protocol for a four-centre clinical trial. BMJ open, 9(5), p.e025701.
Crowfoot, D. and Prasad, V., (2017). Using the plan–do–study–act (PDSA) cycle to make change in general practice. InnovAiT, 10(7), pp.425-430.
Cunningham, C., Peters. K., and Judy Mannix (2013). Physical Health Inequities in People with Severe Mental Illness: Identifying Initiatives for Practice Change, Issues in Mental Health Nursing, 34(12), pp.855-862
Dunn, V., (2017). Young people, mental health practitioners and researchers co-produce a Transition Preparation Programme to improve outcomes and experience for young people leaving Child and Adolescent Mental Health Services (CAMHS). BMC health services research, 17(1), p.293.
Kumah, E., Ankomah, S.E. and Antwi, F., (2016). The role of first-line managers in healthcare change management: a Ghanaian context. International Journal of Biosciences, Healthcare Technology and Management, 6(3), p.20.
McLaughlin, J.E., Bush, A.A., Rodgers, P.T., Scott, M.A., Zomorodi, M., Pinelli, N.R. and Roth, M.T., (2017). Exploring the requisite skills and competencies of pharmacists needed for success in an evolving health care environment. American journal of pharmaceutical education, 81(6). pp.23-34
Mishkind, M., SPHR, S., Waugh, M. and Hubley, S., (2018). Evidence base for use of videoconferencing and other technologies in mental health care. Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals, 31. pp.90-123.
Morain, S.R., Kass, N.E. and Grossmann, C., (2017). What allows a health care system to become a learning health care system: results from interviews with health system leaders. Learning Health Systems, 1(1), p.e10015.
Moussa, L., Garcia-Cardenas, V. and Benrimoj, S.I., (2019). Change Facilitation Strategies Used in the Implementation of Innovations in Healthcare Practice: A Systematic Review. Journal of Change Management, 19(4), pp.283-301.
Mugisha, J., De Hert, M., Stubbs, B., Basangwa, D. and Vancampfort, D., (2017). Physical health policies and metabolic screening in mental health care systems of sub-Saharan African countries: a systematic review. International journal of mental health systems, 11(1), p.31.
Sligo, J., Roberts, V., Gauld, R., Villa, L. and Thirlwall, S., (2019). A checklist for healthcare organisations undergoing transformational change associated with large-scale health information systems implementation. Health Policy and Technology, 8(3), pp.237-247.
Teixeira, B., Gregory, P.A. and Austin, Z., (2017). How are pharmacists in Ontario adapting to practice change? Results of a qualitative analysis using Kotter’s change management model. Canadian Pharmacists Journal/Revue des Pharmaciens du Canada, 150(3), pp.198-205.
Thomson III, N.B., Rawson, J.V., Slade, C.P. and Bledsoe, M., (2016). Transformation and Transformational Leadership:: A Review of the Current and Relevant Literature for Academic Radiologists. Academic radiology, 23(5), pp.592-599.
Wagner, J., (2018). Leadership in Quality Management and Safety. Leadership and Influencing Change in Nursing.
Wickrama, K.A., Klopack, E.T., O’Neal, C.W. and Neppl, T., (2020). Patterning of midlife marital trajectories in enduring marriages in a dyadic context: Physical and mental health outcomes in later years. Journal of Social and Personal Relationships, p.0265407519899726.
Yeomans, D., Dale, K., & Beedle, K. (2014). Systematic computerised cardiovascular health screening for people with severe mental illness. The Psychiatric Bulletin, 38(6), pp.280-284.
Young, S.J., Praskova, A., Hayward, N. and Patterson, S., (2017). Attending to physical health in mental health services in A ustralia: a qualitative study of service users’ experiences and expectations. Health & social care in the community, 25(2), pp.602-611.
Žibert, A. and Starc, A., (2018). Healthcare organizations and decision-making: leadership style for growth and development. JAHS, 4(2), pp.209-224.
Appendix 1:
The benefit of using transformational leadership is that it allows a collaborative work environment to be established where the leaders work along with their subordinates and staffs allowing them to present their opinions and ideas regarding creating any change in business. Thus, the development of purposeful working environment along with value towards the employees by the leaders makes the staffs involved in the change have increased zeal to show work efforts in making the change successful (Žibert and Starc, 2018). Therefore, the transformation leadership is to be used in the change as it would lead to create a collaborative work environment where leaders and staffs would work together and have a common cause towards making the change. However, the limitation to be faced in using transformational leadership is that the leaders may be intended to take wrong decision towards making any aspect of the change (Boamah et al. 2018). This is because the leaders in this style of management are found to be dependent more on the staffs to share ideas and approaches of change rather than use their own skills and opinions in developing ideas of change. Therefore, leaders making the change are to develop effective analysis of the consequence of any suggested idea to be implemented for making the proposed change so that any wrong decision is avoided.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



