The Imperative of Good Mental Health
Introduction
Good mental health is crucial for various reasons. First, it determines a person's physical health. Secondly, it ensures a suitable progression of efforts in developing and maintaining family relationships and healthy people who are crucial resources in the growth and development of the community as a whole. Since mental health affects all components is a person's life, it is thus the responsibility of every stakeholder to ensure that every person develops and maintains good mental health. Additionally, those seeking healthcare dissertation help should consider how mental health factors influence overall well-being and community health initiatives.
On a broader perspective, mental wellbeing is described as not just the state of not having a mental disorder, but a situation where an individual can realize their potential in life. This individual can cope the stressful situations in life, can work productively to meet desired goals, and can make a positive contribution to their community at large (World Health Organisation, 2019).
The World Health Organisation (WHO)'S description of mental wellness depicts the subject as a significant area of human wellbeing. Even though the issue has been of greater importance, the approach to which it is considered is way different and does not match the status of an urgent priority. This involves the prevention and promotion of good mental health among people; these two approaches have been promoting inequality among people in the UK (Government, 2011).

After an in-depth evaluation of physical health, many experts argue that there is an increasing need for recognising the impact of mental health in communities. In the UK, mental health represents 24% of the total ill-health burden and the leading cause of disability among patients (WHO, 2017). These figures show how serious mental health is in the national economy.
In many areas of health, there are distinct inequalities among people from various social backgrounds such as age, ethnicity, and gender with regards to their mental health. Persons from these diverse backgrounds have different capabilities to access mental support and to engage in communities for their mental wellbeing. This disparity makes some disadvantaged groups more vulnerable to mental problems.
Realizing the effect of risk exposure and defensive mechanisms associated with the circumstances of different persons is essential in devising policies aimed at improving mental wellbeing (Chenore et al., 2013). Currently, the government has initiated various commitments to ensure every individual, regardless of their social status, can receive equal opportunities for mental wellbeing (Johnson, 2018). Some of these initiatives include improving physical health, which in turn affects the life expectancy, increasing educational awareness opportunities, introducing better skills, improving employment opportunities and productivity among people, adding various amenities that enhance social interaction among other factors.
Tackling the concerns mentioned above for the entire population will significantly reduce the inequalities existing in mental health and also avert the progression of more serious mental health conditions.
In the economic context, the government commits 11 percent of the annual health budget to mental health (Department of Health, 2019). Over £2 billion is spent on providing social care for the mentally ill people nationally. There is an increase in population and, more specifically, the old generation, which could see the doubling of these costs in the future (Department of Health, 2019).
The effect of mental health in people's lives could not only be associated with health-related costs only but also in their educational achievement, employment, family relationships, among other aspects. The costs related to the issues mentioned above cannot be quantified; however, detailed estimations identify that about mental health issues cost the economy about £105 billion, out of which £30 billion are related to employment (Center for Mental Health, 2019). In this regard, work-related costs arise due to sickness and absence at work and decreased efficiency.
This Health Needs Assessment report focuses on the New Devon Clinical Commissioning Group, which regulates healthcare in the East, West, and North Devon community. The locality under study are towns in Devon County Council located in Southwest England. This submission ascertains that health needs for the local people are changing, and so should the service providers to meet the increasing demand.
The local area
Population
Devon country has an estimated population of 1, 200,000 people who live in the cluster of Devon, Plymouth, and Torbay (Office for National Statistics, 2018). Figure 1 below shows the population by age and gender in comparison with the UK's population. The statistics show that older people are quite many compared with young people. Besides, the female population life expectancy is higher as compared to males in the older generation (see figure 1).
Figure 1 shows population statistics for Devon County, Plymouth, and Torbay in 2011
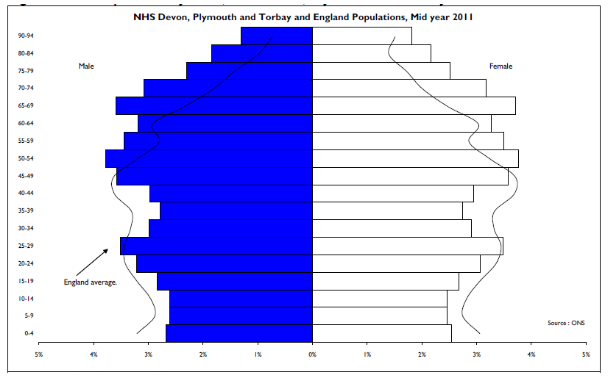
Devon County is split into two clinical commissioning clusters, namely East, West, and North Devon and Torbay, with a population of approximately 900,000 and 300,000 (Office for National Statistics, 2018). The new Devon Clinical Commissioning Group (New CCG), which consists of East, West, and North Devon, has a noticeably older population as compared to the national statistics and is famous for in-migration for retirement age (Office for National Statistics, 2018). Devon has a geographical area coverage of 2,330 square miles, and it includes several smaller towns, villages, and rural parts and a national park (Dartmoor), which is 369 square miles (New Devon Clinical Commissioning Group, 2017).
Commissioner of services
Both physical and mental health services in the North, East, and West Devon are commissioned on behalf of the local people by the New CCG alongside the National Health Service (NHS) and Plymouth City Council, which administers in South Devon. The Commissioner is one of the largest in the UK in the size of the population it commissions. In the 2016/17 report, the total health and social care among East, West, and North Devon amounted to £2 billion, out of which 6% was spent on mental health care (New Devon Clinical Commissioning Group, 2017). The mental health costs only included the amount given to medical providers and not the amount spent on physical needs (NHS, 2020).
Providers of services
The New Devon Clinical Commissioning Group (New DCCG) report shows that there are around 5.5 million consultations at General practitioners in surgery, 850,000 contacts with the community workforce, and 200,000 turnouts at Accident and Emergencies. The locality involves a wide range of institutions that provide health and social services (see image below) (New Devon Clinical Commissioning Group, 2017).
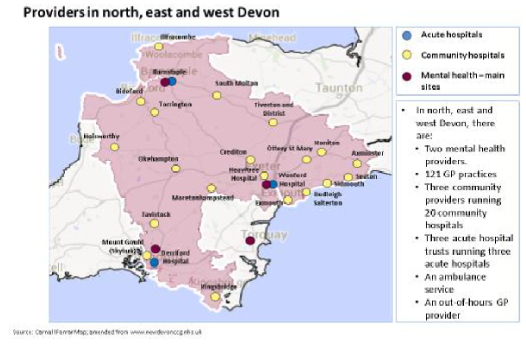
The locality has 121 general practitioner practices, 130 dentist systems, 200 dispensaries, 113 opticians, and several voluntary and community area groupings that are all run independently and offer various services (NHS, 2020).
The locality has only three mental health service providers who offer inpatient mental health services, community health groups, liaison psychotherapy, and other various mental health specialist services. These service providers include
1. Devon Partnership NHS Trust- the organization, provides mental health services across Devon and also in the broader region of Devon County.
2. Plymouth Community Healthcare- this organisation offers mental health services, physical health, both children and adult social care in Plymouth and West Devon.
3. Virgin Care- this organisation offers children and family health, social care services, and community-based mental health services for kids and youths in East, West, North, and South Devon.
Ethnic dispersion
There is a relatively small proportion of ethnic minority groups in Devon as compared with the national population. The 2011 Office of National Statistics highlights that 2.5% of the Devon population represents non-white ethnic groups (Office for National Statistics, 2018). The Asian/Asian British community is quite significant in Devon, representing 1.2% in Devon.
Deprivation
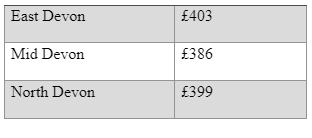
The overall deprivation levels in Devon county are slightly lesser than the national average (see table 1). The most deprived is north and mid-Devon, especially in towns and some market towns.

Several authors and publications have been made before this submission. For instance, the Royal College of Physicians (RCP) highlighted the significance of public mental health, more particularly the identification and intervention in the early stages of the life-course (Royal College of Psychiatrists, 2010). The publication also examines the application of universal and directed strategies to preclusion and how the policies should be employed in the population at large. The report also points to the significance of dual diagnosis as a strategy of ensuring an accurate diagnosis. Further, the RCP report also emphasizes the necessity of involving the service providers in the commissioning of services to make sure the need is ascertained and met. Besides, this involvement also identifies the need for commissioners to deliberate on the impacts of mental health and mental illness across the life course of an individual and even the broader economic effect of enhancing positive mental health and wellbeing.
Another relevant publication is the mental health and wellbeing assessment report 2013 conducted by Priestley on behalf of the Devon County Council (Kirsty Priestley, 2013). The needs assessment report was developed to support the commissioning of mental health and wellbeing services in the clusters of Devon, i.e., East, West, North, South Devon, and Torbay, which will also complement the Plymouth mental health assessment report. The publication also deliberates the broader wellbeing of the county’s population that supports the local authority’s obligation for providing and maintaining public mental health services.
The health needs
Children and young people
The children and youths in the UK represent the country's most susceptible people with mental health problems. These population's mental health and wellbeing are quite crucial in the future health, prosperity, and wellbeing of society (McGorry et al., 2013). Behavioral and emotional problems, especially in the early stages in life, are predictors of mental health problems in later stages. Therefore, a positive parent-child association is crucial in the emotional and behavioral development of a child. Besides, the extent to which a parent interacts with their children and how negative it accounts for approximately 35% of the anti-social behavior variation in young people (Patterson et al., 2017). Thus, parent's desires and family settings are significant contributors to children's mental health and, indeed, the life chances of young people.
Both children and youth and their families possess distinct levels of needs, and they often change over time, contingent on their situations. Thus any evaluation should consider the entire family needs.
Several known factors make young people and families most vulnerable to mental problems. The children at risk for this problem are those born with low weight, those with deprived child-parent attachment, and those with weak cognitive, social, and emotive capabilities or those who have interactive problems (Johnson, 2018). In older youths, contributing factors include family troubles, transition into adulthood, teenage pregnancy, and lousy influence from peers. The mental health among children and teens is a multifaceted aspect. If the stakeholders desire to improve mental wellbeing, they should look into the factors and risks contributing to poor mental health and also protect those that affect mental wellbeing. At this stage, early involvements, including self-esteem development activities and improvement of child-parent relationships, are crucial in addressing the mental health needs of young people (Moffitt, 2017).
Devon has higher rates of self-harm in teenagers as compared to anywhere else in the Southwest part of England. For instance, the schools have concerns with drug use while some parents complain of their kids being cyber-bullied on social media (Clark, 2018). According to Clark (2018), cyberbullying is one of the leading problems causing self-harm among children. Social media is also believed to expose young people to body-image pressures, which might lead to unrealistic personality goals, such as becoming celebrities (Moffitt, 2017).
Domestic violence is also another most prevalent concern attributed to young people's emotional and mental wellbeing. Children and teenagers from backgrounds with parents who usually engage in violence are more likely to develop emotional problems in their later stages of life (Patterson et al., 2017). BBC report in 2015 shows that incidences of domestic violence continue to increase in Devon County; for instance, in 2010, there were 2,190 reported cases as compared with 2,502 cases in 2014 (BBC, 2015). Besides, approximately 55% of the reported cases are associated with alcohol and drug abuse.
Gender identity
Transition into adulthood is another aspect that determines the mental health and wellbeing of a Child (Moffitt, 2017). According to Clark (2018), secondary schools in Devon recorded that gender identity is among the issue that influences emotional health and wellbeing of a teenager. In this regard, most teenagers are eager to explore their gender identity (Moffitt, 2017).
Transitioning from childhood to adulthood can be a challenging process for children in primary schools. While some schools have good buddying policies that support year seven students, including counseling, there is much concern of situations where a child comes from a small cohort of pupils to a much larger secondary school and become overwhelmed by peer pressure (Clark, 2018).
Emotional health and wellbeing among young people, especially in rural areas of East, West, and North Devon including Barnstaple, and North Leigh, might sometimes be unseen. For boys, there can be an internalisation of mental health needs who might not have an outlet to express their emotions and feelings, which might result in suicide. In Devon County, there is a higher prevalence for male students to commit suicide than females in schools (Clark, 2018). Besides, in some schools, pupils log anonymously in mental support facilities and perceive it as a useful tool for conveying concerns (Moffitt, 2017). Therefore, managing the transition process from childhood to adulthood is a primary challenge in Devon county schools, and what matters is the cultural change in the institution and implementation of measures that promote the mental wellbeing of the children and youths (McGorry et al., 2013). However, the fact remains that most of these pupils are more likely to succeed when the schools get it right for their most vulnerable students.
Autism
The Devon County Council Task group of 2013 sought to determine the Children & Young People's Emotional Health & Wellbeing in Devon County schools (Children’s Scrutiny Committee, 2013). The task group notes several reports of pupils joining schools at year seven who usually have undiagnosed autism. These kinds of children typically are labeled as naughty, when in the real sense, they have an Autistic Spectrum Disorder (ASD). Therefore most schools need to identify barriers to learn what the children have. Whereas these pupils are on the waiting list, several other children are being referred to the County Council for a reason being the child cannot attend school (Clark, 2018). Even though the county council has identified approximately 100 centers where such pupils can receive medical tuition, the waiting list for the autism evaluation process is a bit long (taking up to a year) (Children’s Scrutiny Committee, 2013).
Old age people
The majority of users of hospitals and care homes in the UK currently are older persons (Berzins et al., 2018). A report by Imison et al. (2012) finds that people over 62 years and above account for over 62% bed occupancy in the hospital and 68% of emergency bed occupancy days. And this number is expected to increase with the increasing number of older people nationally (Imison, 2012). Besides, the average length of stay in beds at the hospital is approximately eight days for people aged between 65-74 years, ten days for persons with the age of 75-84; and 12 days for patients above 85 years (Vilches-Moraga et al., 2017). For instance, in the eastern locality of Devon, 50% of emergency admissions in the hospitals were accrued to patients at the age of 65 years and above (New Devon Clinical Commissioning Group, 2017).
The needs for mental and social care keep growing, and the available amenities for these challenges are fewer causing a significant problem for commissioners and service providers in the locality of East, West, and North Devon. Even though the number of people with long-term conditions is projected to become relatively stable in the next 6 to 8 years, the number of multiple long-term conditions commonly referred to as multi-morbidity is expected to increase by 17% by 2022 Kingston et al., (2018).
The system's ability to provide the needed range of mental and health care along with the increasing demand could also become ineffective by the future workforce capacity and capability. A projection by the Royal College of Nursing (2011) indicates that most professionals who will be working in health and social care by 2022 are still the same people working in the same setting today. In this regard, the future workforce configuration shows a potential shortfall of approximately 70,000 nurses in 2022. Also, the increasing number of adult patients necessitate an increase in the adult social care employees by a total of one million professional by 2025 if existing service configurations remain unchanged.
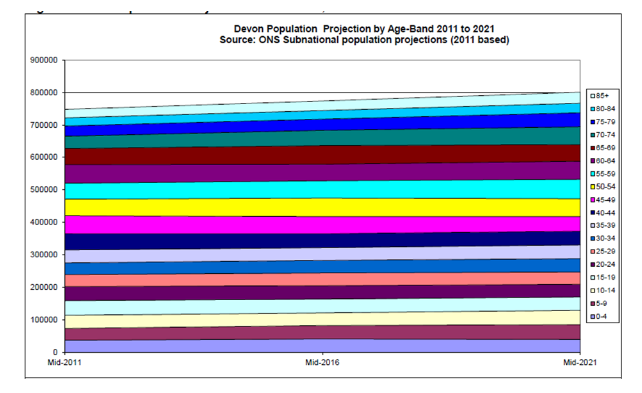
The New Devon Clinical Commissioning Group has particular challenges regarding the aging population. The Office of National Statistics projects a higher proportion and growth among old age groups, especially the 70 and above group by 2021 in Devon County (see figure 2 below).
An inspection carried out by the Care Quality Commission in 2018 on Devon's vital adult mental health services reveals a mixed picture of care from being outstanding to being inadequate (Merritt, 2019). Most concerns point to the high-risk and urgent patients waiting for a year instead of a maximum of a week for treatment. The report also finds that other patients wait up to three years, and the number in the waiting lists keeps soaring.
Between March 2018 and February 2019, the report indicates that 400 patients had received treatment out-of-bed since there were not enough beds, which shows an increase of 89 patients from the last inspection (Merritt, 2018). Some adults of working age were receiving treatment from the wards of older people with mental health illnesses because of the same challenge. The report also finds that the community mental health groups for adult patients could not provide treatment to all patients within the required 18-week referral to treatment time. Lastly, the waiting time for the ASD patients and Attention Deficit Hyperactivity Disorder (ADH) was still very long at the facilities. From this report, it is reasonable to note that the mental health care services at East, West, and North Devon require improvement.
Current interventions
Currently, various facilities in the locality offer high-quality services each day and might continue being so in the coming days. The National Health Service and the New DCCG have, in previous times, had several achievements creating a transformation to the local services and delivering needs to the local people. There are also various projects that these players have already implemented; some of them are listed below.
Early Help
Since 2015, the Devon County Council has implemented a program that delivers interventions to troubled families and children intending to provide support and build resilient families. The motivating factor for this intervention was the surrounding anti-social behavior among children, absenteeism in schools, joblessness, and extensive agency concern. The County Council has since established locality groups that manage and deliver these intermediations to families via a multi-agency approach. The County Council's efforts are its first attempts to join private agencies that habitually consult with distressed families into a sole mutual service (Policy, 2019). These interventions have assisted in the transformation of local health and social care systems to adapt to providing better services for the local people. However, a lot still needs to be done to satisfy the local needs and continuously deliver the highest quality of care to make sure value for money.
SMART Recovery program
In 2015, the Devon Partnership Trust set an ambitious four-year plan called the SMART recovery. The program combines the care pathways, mobile working, and more efficient utilisation of estates to enable staff to reduce the time spent in commuting to service delivery points and provide more time in care provision (Ross & Naylor, 2017). The program is a transformational action that has made service usage easier through the creation of a single 'front door' for care. The operation points for the trust have been reduced while the staff has been provided with new capable equipment that enables the provision of care efficiently. Also, the program aims at setting up care hubs in surrounding regions, especially in South Devon and Torbay (Barrett et al., 2017).
The needs of local people
Citizens in the East, West, and North of Devon have distinct health and social care needs. Some of them require intensive support, for instance, patients with dementia-related symptoms, while those with mild cognitive symptoms such as anxiety require social care services infrequently (Hollis et al., 2017). Much of these needs depend on the extent of the illness people have and the level of care they need. In efforts to comprehend these needs, it is crucial to look at various requirements for the people at the locality.
The local people have high expectancy rates, and so they need long-term care
For instance, the ratio of young to older people (65 years and above) in East, West, and North Devon is 1:5 which is higher than the national average, which stands at 1:4 (ONS, 2011). Besides, the number of older people (over 85 years) is also high, standing at 3.1% as compared with the national average of 2.3%. The East of Devon has higher numbers than the West, but all these areas are experiencing an increase, which is similar to the national average growth.
An old generation implicates increased cases of dementia-related symptoms, which requires long-term care. For instance, in 2015, Northern, Eastern, and Western Devon CCG had the most people living with dementia, at 15,487 (Alzheimer's Research UK, Dementia Statistics ). Over 2 in every five admitted patients over the age of 70 years who receive emergency admission are patients with dementia symptoms.
In addition to dementia-related symptoms are other mild mental illness symptoms such as depression and anxiety. For instance, over 200,000 people between 18-64 years have been diagnosed with a mental disorder such as depression and anxiety. While the number of dementia people stands at 15,487, 1,200 children have been diagnosed with mental illness such as schizophrenia (Hayes et al., 2017).
There is a challenge in the locality because people with serious mental illness are three to four times more likely to die from the disease than the general population ( Public Health Outcomes Framework, 2018). Besides, evidence suggests that people with mental illness are more likely to have poor physical health (Scott et al., 2017). For instance, a person who has depression is more likely to develop coronary heart disease. At the same time, they also have worse survival rates from cancer and heart diseases (Royal College of Psychiatrists, 2010). The locality has higher rates of depression as compared to other areas ( Public Health Outcomes Framework, 2018). The report also ascertains that the amount spent on mental health in East, West, and North Devon is less than in other areas. Mental illness is prevalent in the North, East, and West Devon, and therefore mental health care must be given equal attention to physical health. In this regard, discrimination on mental illness among people in various backgrounds should end, and patients should receive the needed support whenever they require.
Over 45% of bed occupancy in Devon County facilities has people with dementia who are medically fit to leave the facility but have not been discharged (Devon County Council, 2018). Provided that various people are living with dementia in the locality, there is a sufficient opportunity for the service providers and Commissioner of services to develop world-class facilities to meet the needs.
From these shreds of evidence, it is reasonable to argue that local health and social care in this locality need to prioritize high quality and accessible services for persons with mental disorders, especially those who have poor physical health. Besides, the services also should prioritize mental health among people with a physical health need.
Future local interventions
The above successes show that young people and children in East, West, and North Devon know where to go and find help within schools. Besides, the centers built by the County Council ensure confidentiality, which motivates young people to seek help. However, it is ascertained that more work still needs to be done within schools to explore the emotional status and wellbeing of students, especially those with ASD. This approach will raise awareness of services locally to seek information, guidance, and support. In this regard the Devon health watch should;
Establish a stout organized model to make sure that the voices of children and youths are heard by the commissioning authority and also the emotional healthcare service providers in the locality. The Devon County Council could make this happen by building sub-centers within schools where students could visit to receive mental healthcare. Besides, the sub-centers will make the services more accessible, and urgent help could be provided when needed.
Secondly, the emotional wellbeing advice and support process should be confidential for those children and youths who are having emotional problems. The County Council can implement this policy by ensuring schools have a school counselor or nurse who could ensure that students' need is met and kept in privacy. Besides, the school nurse could signpost the student to other services, including peer support groups, if the need arises.
Third, information relating to emotional wellbeing services could be made available in schools, community facilities, among other places. This approach will inform young people where support and advice are provided; this action would ensure many young people are well aware of the accessibility of the services. Besides, young people could also be involved in the planning of the publicity to ensure it appeals to many. Also, information regarding peer support groups and support networks should be made locally for the schools, statutory and community to access it easily.
The youths and children should also be encouraged to offer feedback regarding the service they receive at various points. This way, monitoring, and evaluation could be done to make processes easy and attractive to the visitors.
It is therefore recommended that the stakeholders in the locality should continue doing a health watch to provide support and advice to children and young people in their emotional wellbeing. Besides, it is also reasonable if they could monitor the results of the recommendations made in several reports produced for this course.
Quick discharges
When patients visit the hospitals, they tend to stay longer than expected even after being declared fit to be discharged. This is because when the patients are ready to leave, the local services are not prepared to look after them, and this makes them stay much longer at the hospital. The waiting period is generally for seeking health services in their homes, a bed in a community facility, or for packages of social care (Royal College of Psychiatrists, 2010). These amenities are mostly not capable of accepting transfers or setting up care packages during weekends, so individuals who have been declared fit are stuck in facilities.
These people are exposed to several implications while at the hospital, they might develop other complications due to the nature of the healthcare facility. Besides, delays in discharge play a part in a poor experience in service delivery and might cause a long-term adverse effect on independent living. Also, the longer stays at hospitals imply poor value for money since the services at the hospital are not being provided efficiently. It is recommended that the Commissioner of services should focus on improving community services so that people should leave hospitals whenever they should.
Retaining and hiring sufficient workforce
Better and high quality of services depends on how well a nurse is trained, motivated, and experienced. Besides, a well-motivated staff increases the quality of care hence improving the client experience (Chenore et al., 2013). Unfortunately, in East, West, and North Devon, the workforce have various issues, which makes it hard to provide high-quality services to increase patient experience. For instance, the facilities have an aging workforce, which is a challenge since the National Health Service and social care lose experienced and well-trained staff when they retire. One out of three general practitioners and two out of five nurses in practices at East, West, and North Devon hospitals are over the age of 50 (NHS, 2020).

Given that the facilities have an aging population, it is tremendously crucial that the County Council retain well-trained staff. The inadequate experienced workforce in the facilities means that the quality of healthcare services will not be afforded to the local people today and even in the future.
Conclusion
East, West, and North Devon are localities under the New CCG, which is a commissioner of health and social care services in the region. Mental health care in these localities is experiencing difficulties, especially with the increasing number of patients and changing demands in the sector. The children and young people have various needs, especially with their transition from childhood to adulthood. Besides, the family backgrounds from which the young people grow in has a significant influence on their emotional wellbeing. Additionally, the locality has a large elderly population who need long-term healthcare; unfortunately, there are no sufficient workforces to meet all these demands in the future. The facilities have an aging workforce, and there are no robust measures to retain well-trained and experienced personnel.
The patients stay longer in the hospitals even after being declared medically fit to leave the facilities. Therefore, local health and social care services cannot continue operating this way. They need to develop robust measures to ensure young people and children's demands are met. And this undertaking should involve getting emotional wellbeing services closer to them and engage them in all actions of the processes. Besides, the local service should implement better policies to ensure it retains and attracts well-trained professionals to meet the current and future demands of the patients.
A lot can be learned from this locality, especially on how it delivers its services, for instance, it is clear that the needs of local people are changing and so the health and social care delivery also need to change. Changes in health are inevitable, and they always relate to service delivery; therefore, it is expected that all stakeholders should provide their clients value for money.
It is expected that this work would benefit the local policymakers by informing them that the public is aware and concerned about service delivery and need value for money. Besides, it would help them in conducting further research on the locality’s health needs and find other options to better the health system.
Continue your exploration of The Impact of Work on Health with our related content.
References
- Barrett, J., Aitken, P., & Lee, W. (2017). Report of the 2nd annual survey of liaison psychiatry in England. Royal College of psychiatrists. Royal College of psychiatrists.
- BBC . (2015). Domestic abuse reports rise in Devon and Cornwall. BBC News .
- Berzins, K., Baker, J., Brown, M., & Lawton, R. (2018). A cross‐sectional survey of mental health service users’, carers’ and professionals’ priorities for patient safety in the United Kingdom. Health Expectations, 21(6), 1085-1094.
- Chenore, T., Pereira Gray, D. J., Forrer, J., Wright, C., & Evans, P. H. (2013). Emergency hospital admissions for the elderly: insights from the Devon Predictive Model. Journal of Public Health, 35(4), 616-623.
- Clark, D. (2018). Self-harm, drug use, and cyber-bullying among issues facing teenagers in Devon schools. Devon Live .
- Government, H. M. (2011). No health without mental health: a cross‐government mental health outcomes strategy for people of all ages.
- Hayes, J. F., Marston, L., Walters, K., King, M. B., & Osborn, D. P. (2017). Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000–2014. The British Journal of Psychiatry, 211(3), 175-181.
- Hollis, C., Falconer, C. J., Martin, J. L., Whittington, C., Stockton, S., Glazebrook, C., & Davies, E. B. (2017). Annual Research Review: Digital health interventions for children and young people with mental health problems–a systematic and meta‐review. Journal of Child Psychology and Psychiatry, 58(4), 474-503.
- Imison, C. (2012). Future trends. Kings Fund, 2.
- Imison, C., Poteliakhoff, E., & Thompson, J. (2012). Older people and emergency bed use: exploring variation. King's Fund.
- Johnson, R. (2018). Are we nearly there yet?.
- Kingston, A., Robinson, L., Booth, H., Knapp, M., Jagger, C., & MODEM project. (2018). Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age and ageing, 47(3), 374-380.
- McGorry, P., Bates, T., & Birchwood, M. (2013). Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. The British Journal of Psychiatry, 202(s54), s30-s35.
- Moffitt, T. E. (2017). Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. In Biosocial theories of crime (pp. 69-96). Routledge.
- New Devon Clinical Commissioning Group. (2017). Clinical Policy Committee - Annual Reports. New Devon .
- Patterson, G. R., DeBaryshe, B. D., & Ramsey, E. (2017). A developmental perspective on antisocial behavior. In Developmental and life-course criminological theories (pp. 29-35). Routledge.
- Policy, A. (2019). Admissions policy. Policy.
- Ross, S., & Naylor, C. (2017). Quality improvement in mental health. King's Fund.
- Royal College of Psychiatrists. (2010). No health without public mental health: The case for action.
- Scott, K. M., Lim, C., Al-Hamzawi, A., Alonso, J., Bruffaerts, R., Caldas-de-Almeida, J. M., ... & Kawakami, N. (2016). Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA psychiatry, 73(2), 150-158.
- Vilches-Moraga, A., Fox, J., Paracha, A., Gomez-Quintanilla, A., Maevis, T., Epstein, J., & Thomson, A. M. (2017). Baseline characteristics and clinical outcomes of older patients admitted as an emergency to general surgical wards. Salford-POPS–GS. European Geriatric Medicine, 8(5-6), 499-504.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



