Understanding the Rising Prevalence of Obesity in Suffolk
Abstract
Introduction
Obesity is a health condition in which excess fat is accumulated in the adipose tissues thereby increasing the Body Mass Index (BMI) [more than 30 kg/m2] (Muttarak, 2018). The body mass index of a person is measured by dividing his or her body weight by the square of a person's height. In East England, the prevalence of obesity in adults increases at a faster rate thereby posing serious health implications on the health and wellbeing of the population. For those researching this area, seeking healthcare dissertation help can provide deeper insights. Obesity is associated with many chronic illnesses such as cardiovascular disease (CVD), coronary arterial disease, musculoskeletal disease such as arthritis, a pulmonary disorder, hypertension, type 2 diabetes and cancer (Gregg et al. 2017). This study has selected Suffolk, the country that is located in East of England [EOE], to discuss the prevalence of obesity in this locality. This country is selected for the topic because this country is reported to have a high rate of obesity in adults that enhance their vulnerability to different chronic illness such as diabetes, pulmonary illness ad CVD. In recent year, more than 62% of adults in England suffer from obesity and overweight. Recent reports show that in Suffolk, the obesity in adults (18+) that has been registered to the GP practices increases from 10% in 2018 to 11.5%in 2020.

In this context, the selection of this locality is highly appropriate to highlight the importance of taking an effective health promotion initiative to reduce the prevalence of obesity in the adult population in Suffolk. This study will discuss the health and social care data of Suffolk to discuss the current social and healthcare status in relation to obesity in adults. Additionally, the study will also evaluate the determinants of obesity in Suffolk such as health inequalities, nutrition, socio-economic condition and lifestyles in this locality. Finally, the study will discuss the current service provision and the nurse’s roles in health promotion and screening to protect adults from the high prevalence of obesity.
Locality: East of England, Suffolk:
Suffolk is a historic country in East England. It is bordered by the North Sea in the East, Cambridgeshire in the West, Essex in the south and Norfolk in the North. This administrative country of seven districts. It has a wide variety of landscape. The major of the economy in this country is agriculture (healthysuffolk.org.uk, 2019). It as well-known agricultural firms such as Benson Pickle and Great King, despite having a growing economy, this country is reported to have incomes inequality and health inequalities. Many people reside in the below poverty level, therefore, are devoid of proper nutrition, high-quality foods, education, healthcare facilities and health education. In recent years. Obesity and overweight in the adult population due to health inequality has become a major challenge for Suffolk that cost a high amount to the NHS England each year thereby posing adverse impacts on the overall economy of England [PHE, 2020].
Health and social care data:
Obesity in adults has become a major health concern in Suffolk in recent years. The JSNA report (2019) shows that, in 2017/18, 6 out of 10 adults were diagnosed as obese in Suffolk. Waveney locality of Suffolk shows the highest prevalence of obesity in adults in which 7 out of 10 adults are obese. As mentioned by Wilding et al. (2020), obesity and overweight in adults make them highly vulnerable to the risk of mortality and morbidity.
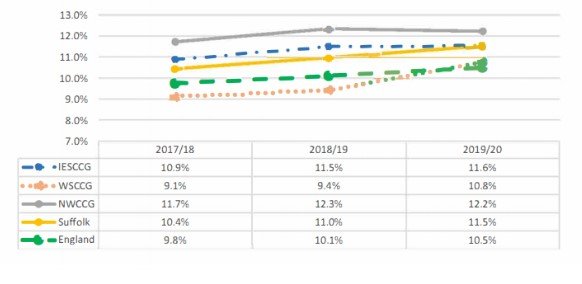
From the above-mentioned NHS database, it is seen that the risk of obesity in the 18+ population increases in each year from 10.4% in 2018 to 11.5% in 2020 (healthysuffolk.org.uk, 2019). This rate is higher than that in England (10.4% in Suffolk as compared to 9.8% of England)
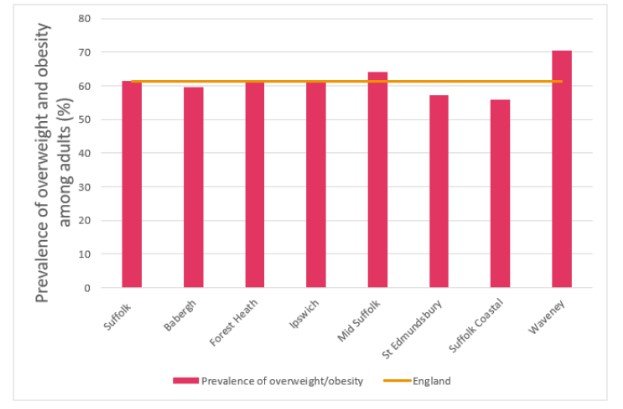
The above-mentioned graphical presentation shows that more than 60 % of adults are vulnerable to the risk of overweight and obesity. Year Lived with Disability (YLDs) is the parameter that is used to measure the overburden of obesity and other diseases in the locality. In the case of Suffolk, the YLDs is 7780 years, which shows that residents of this locality live with different health conditions for several years, which enhance the numbers morbidity rate in this country (www.ons.gov.uk, 2020). Obesity and overweight are proved to be the potential cause of the majority of heart attack and CVD in Suffolk. Evidence suggests that high BMI rate (more than 25kg/m2) in most of the adults in Suffolk contribute to developing different health issues such as high plasma glucose, arterial blockage by accumulation plaque and narrowing of the pulmonary artery (Hamer et al. 2019).
There are wide ranges of a health complication that are associated with obesity (Croker et al. 2020). In the Suffolk adult population who are obese are 5 times more likely to suffers from a long-term illness such as type 2 diabetes, heart stroke, heart failure, cardiac disorders, pulmonary illness, hypertension and breathing issues (George et al. 2017). The JSNA report if Suffolk also shows that obesity in adults is 3 times more likely to suffer from the Colon cancer that increases the obesity-triggered mortality in adults (www.healthysuffolk.org.uk, 2019).
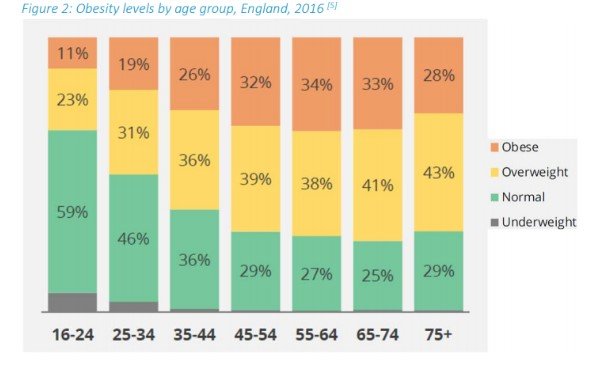
From the graphical data of PHE (2019), it is seen that in England the occurrence of obesity is directly proportional to the age in which the rates of obesity is highest at the age group 55-64. As mentioned by Cherla et al. (2020) there is a strong association between obesity and age. The PHE (2019) report shows that in England the prevalence of obesity increases with the increasing age in people and the rate is highest above the age of 45. On this note, Suffolk has a high proportion of the ageing population and the majority of them are above 45 years, which is the potential reason behind ever-increasing numbers of adult obesity cases in this country.
The PHE (2019) reports show that the hospital admission of adults due to obesity and overweight has been doubled in Suffolk in the last year [PHE, 2019]. The number of obesity-related hospital admission in Suffolk has bee increased from 734 to more than 1356 in every 100000 adults. The data also shows that, in the majority of the hospital cases, the patients are diagnosed with an additional health condition such as types 2 diabetes and cardiovascular illness that enhances their risk of mortality (healthysuffolk.org.uk, 2019).
There are several determinants of obesity in Suffolk such as
Physical activity (Viner et al. 2020) Genetics Medication (George et al. 2017) Diet Overeating Social issues DisabilityPoor diet and nutrition in Suffolk:
Poor diet is common in East England, especially in Suffolk, which is one of the potential reasons behind the high prevalence of obesity in this locality. As mentioned by George et al. (2017), a healthy diet and good nutrition intake are fundamentals to have good physical, mental and emotional health. PHE (2019), recommends that a good and healthy diet must consist of 5 portions of vegetables and fruits in a day (data.England.nhs.uk, 2019). The PHE data shows that in Suffolk, there is 6 in 10 adults (61.4%) who eats 5 vegetables and fruits in a day and this rate is higher than that in England. However, not all regions of Suffolk have a high proportion of adults who eat 5 a day (www.ons.gov.uk, 2020). In mid- Suffolk, the number of adults eating 5 a day is higher than that of the other parts but in Suffolk coastal region the proportion is lower than that in England.
Despite the impressive rate of adults in Suffolk who eat the PHE recommended diet in Suffolk there are many dietary risk factors such as eating too much junk foods, alcohol consumption and smoking that contribute to developing obesity and overweight them (Hobbs et al. 2019). Recent PHE data shows that due to the consumption of high cholesterol and fat-enriched foods ailing at an early age (below 18) and alcoholism there is an increasing rate of different chronic health condition in Suffolk such as 31% of adults with diabetes risk, 6.4% are with risk of cancer and 42% of adults are with the risk of CVD (healthysuffolk.org.uk, 2019).
The density of different fast-food outlets in Suffolk varies from 54 to 129 in different wards of Suffolk per 1000,000 residents (www.healthysuffolk.org.uk, 2019). This high density of fast-food outlets leads to provoking adults and children in Suffolk to eat different types of junk foods that are enriched with saturated fats and high cholesterol. The PHE (2019) data shows that the highest deprivation areas in Suffolk have a high density of fast-food outlets which makes the adults and children in these poor community get easy access to unhealthy foods [PHE, 2019]. The high density of junk foods in the university, colleges and schools in the deprived areas such as Ipswich and Waveney make it difficult for the resident to have a healthy diet. As mentioned by Agha and Agha (2017), in deprived areas of Suffolk there are many outlets of low quality and cheap junk foods that are not only harmful for health nut also are acaricide with risk of infection to people. PHE (2019), there is strong relation between the deprivation and junk foods, because there are many poor street food sellers who cannot afford the street tax to the local authority on high society areas, therefore they have to sells their food products on the streets of deprived areas (PHE, 2019). This is why the numbers of street food shops are more in the deprived communities as compared to the rich communities (Hobbs et al. 2019)). As these junk foods are cheaper than the other healthy foods, families residing in the deprived areas can easily afford these foods for children to fulfil their hunger which leads to vulnerability of deprived children to obesity. This is why obesity in Suffolk is more severe in the deprived communities as compared to high-class societies. Take a deeper dive into Managing Hypoglycaemia in Diabetic Patients with our additional resources.
Physical activity:
As mentioned by George et al. (2017) regular physical activities are crucial for proper weight management and developing positive health and wellbeing. In Suffolk, most of the adults do not perform any exercise or systematic physical activities that contribute to increasing their weight. Adults who reside in the most deprived areas of Suffolk lived an irregular and lack of systematic lifestyles without any physical exercise. Additionally, the high consumption of unhealthy foods that are enriched with saturated factors and cholesterol leads to the accumulation of access fat into the adipose tissues (Baker et al. 2018.). Lack of physical exercise and systematic lifestyles makes it difficult for the body to remove the excess fats through blood flow. As argued by Hobbs et al. (2019) as compared to the people in the deprived areas, the people residing in the higher societies are more likely to be obese due to their sedentary lifestyles. In Suffolk, the majority of the family residing in the high society areas are not performing minimum exercise in a day as they tend to perform all the work by their servants (Booth et al. 2017). Adults in rich areas also affected by obesity at a high rate because of lack of exercise and high consumption of high fat and protein-enriched foods (Garcia et al. 2017).
Medication:
Evidence suggests that adults which take medicines for additional health conditions are vulnerable to put on excess weight that causes obesity in them (Agha and Agha, 2017). Many drugs cause potential changes in the hormonal system inside the body due to which reduces the secretion of hormones and enzymes that are associated with fat digestion. Therefore, the undigested fats are accumulated into adipose tissue thereby increasing the body weight (Garcia et al. 2017). In Suffolk obesity is very common in the adults residing in the most deprived society because the majority of them take antidepressant medicines to cope up with depression, anxiety and psychotic disorders. These medicines have adverse impacts on the digestive enzymes which enhances the chances of obesity of these adults.
Social issues:
Health inequality:
The socio-economic condition of a person is strongly associated with his or her vulnerability to obesity and overweight, the socioeconomic condition includes education, housing, hygiene, income, health and social facilities, employment and accessibility to healthy foods. In Suffolk 10.5 % of the population residing in the most deprived areas (healthysuffolk.org.uk, 2019). Adults belonging to the most deprived families are more like to develop obesity and other serious illness such as CVD and diabetes due to their lack of access to education, income, employment, healthy foods, health education and social support as compared to their richer peers (Booth et al. 2017).
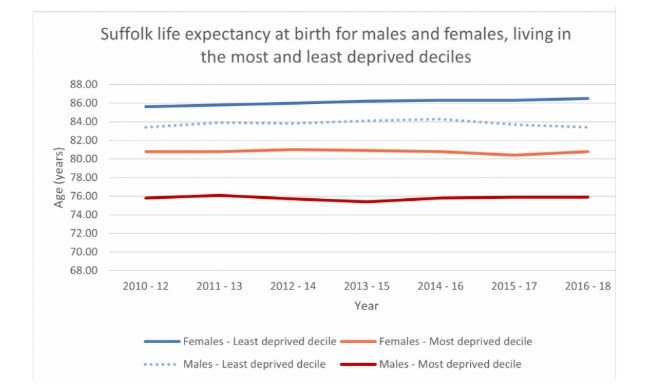
The graphical presentation shows that the life expectancy of the 10 of the males and females residing in the mots deprives areas of Suffolk have less life expectancy rate as compared to the 10% of the males and females residing in the least deprived areas [data.england.nhs.uk, 2019]. In the least deprived areas of Suffolk life expectancy is 63.9 years in the case of males and 65.1 years in the case of male (healthysuffolk.org.uk, 2019). PHE (2019) shows that there is a high gap between health wellbeing and life expectancies due to income disparities in different social class. The PHE (2019) data shows that people residing in the most deprived communities in Suffolk less than 19 years than those residing in the least deprived communities [PHE, 2019]. On the other hand, people residing in the most deprived areas of Suffolk are more likely to suffer from obesity that triggers the risks of other chronic health condition such as CVD, pulmonary illness, colon cancer and heart attack.
Physical disability in Suffolk is more apparent in the most deprived areas in which people are devoid of proper health education, proper social and health care support and good nutrition (Adámek, 2017). As mentioned by Adámek (2017), there is a strong connection between obesity and physical disability. Excess accumulation of fats can make it difficult for people to perform their regular physical activities. The PHE (2019) data shows that in Suffolk 37% of women and 5% of men with obesity in the most deprived areas are more likely to have the chances of developing arthritis and immobility do excess fat accumulation in the adipose tissues the leg muscles as compared to the 21% women and 2% men in the least deprived areas [data.england.nhs.uk, 2019]. As mentioned by poverty plays crucial roles in developing unhealthy habits in people such as smoking, drinking and drug addiction that leads to excess body weight thereby increasing the risk of physical diabolist. In Suffolk, the smoking prevalence in the most deprived area is 42.5% as compared to 13% of the least deprived areas (healthysuffolk.org.uk, 2019). Evidence shows that adults who reside in the poorest communities of Suffolk are more likely to suffer from joblessness and lack of access to a healthy lifestyle as well as a healthy diet which develop unhealthy practices in them such as smoking and alcoholism that can cause several physical health issues such as breathing issues, COPD, cancer, lung infection and CVD that contribute to permanent physical duality (Agha and Agha, 2017).
Biological factors are associated with the socio-economic condition of people. In Suffolk, the adults who reside in the least deprived zone are more likely to have good physical health as compared to the people residing in the poorest areas. This is because the least deprived adults can have a healthy lifestyle, good education, proper healthcare facility, healthy foods and a nutritional diet that improve their biological system (Booth et al. 2017). In Suffolk, the adults residing in the poorest areas get easier availability of unhealthy foods that cause metabolic dysfunction and digestives issues in them. Poor adults in Suffolk are more likely to be habituated to an unhealthy lifestyle such as skipping meals, poor nutritional intake and a fat-enriched diet that cause hormonal disbalance in the internal body function thereby leading to obesity and other serious health issues in them (Booth et al. 2017).
Review of the current services provision:
Local weight loss groups
UK government has set up defence weight management facilities for citizen which can assist the adults in Suffolk to get weight loss training thereby controlling their obesity.
Local service:
Primary care:
Under the primary care services, GPs provide free health check-up and weekly physical health assessment of Suffolk people (Gregg et al. 2017). this clinical supportwould assist the people residing in the deprived communities of Suffolk to get all details on their BMI rate, weight and risk to obesity.
Health service executives (HSE) provide the proper health information to people in Suffolk regarding what is obesity, how it develops its risk factors and its prevention and management (Hamer et al. 2019).
National Mapping of Weight loss services (UK):
Under this process, adults in Suffolk can take weight management training from the local weight management centres. Under this policy, the trainer must provide such training to the service user to manage their weight that will be relevant to their current health condition [PHE, 2019].
GP assessment:
Under NICE guidelines, people with overweight and obesity can take free GP consultation on managing their weight, BMI and height [NICE, 2020]. Under the weight management initiatives taken by the UK government, the adults with obesity in Suffolk can take the facility of monthly check-up of the BMI and weight that will enable them to track that whether they lose or gain weight during undertaking the weight management training.
NHS 12 weeks weight loss plan
Under this plan people will be motivated and trained to have a healthy lifestyle and a highly effective nutritional intake that will assist them to reduces their excess weight (data.england.nhs.uk, 2019). This plan include
Healthy nutritional and dietary policy:
PHE (2019) recommend a dietary ad nutritional policy for tackling the prevalence of obesity in adults in Suffolk (data.england.nhs.uk, 2019). This dietary policy recommends:
Eat 5 a day: adults need to eat 5 vegetables and fruits in a day A base meal such as starchy foods including rice pasta and potatoes need to be eaten Eat some dairy products or dairy alternatives such as soya drinks Eat beans, egg, fish, pulses and meats to meet the everyday demand for protein East unsaturated oils and food with unsaturated fats in fewer amounts
Healthy lifestyle:
This NHS plan s is highly effective for obese adults of Suffolk in terms of bringing about effective changes in their lifestyles thereby promoting their health and wellbeing (healthysuffolk.org.uk, 2019).
Sufficient sleep Early rising and early sleeping Regular exercise No skipping of meals Eat the proper quantity of food Measure that calorie that is intake in a day Use stress management exercise such as deep breathing Improves self-management ability
Roles of the nurse in health promotion ad screening:
Nurses play crucial roles in reducing obesity in the adults of Suffolk.
Under NICE (2019), nurses must play crucial roles in educating patients about obesity, its cause and outcomes of patient’s health [Nobles et al. 2019]. Nurses will provide proper health information of the adults in Suffolk regarding their healthcare system, the function of the body system and high obesity developed through fat accumulation (www.ons.gov.uk, 2020).
Nurses will improve the health literacy of adults by improving their knowledge about what precautions they take for preventing obesity (Adámek, 2017). In Suffolk, nurses play crucial roles in improving their knowledge of people regarding healthy eating, nutrition and good diet and systematic lifestyles that can reduce the obesity prevalence (Pinho-Gomes et al. 2021).
Nurses in Suffolk work in partnership with the obese patient to gain a good understanding of their health choices, food habits, health issues and personal preferences (Booth et al. 2017). This information will assist the nurses to develop and implement an effective care plan for people to prevent obesity in them

Conclusion:
From the above-mentioned discussion, it can be stated that obesity is the health condition in which excess fat is stored into the adipose tissues of the muscles thereby increasing the BMI. Suffolk, the East England country, has high rates of obesity in the adult's population. The determinants of obesity in Suffolk are health inequalities, unemployment, poor housing facilities, lack of income and lack of systematic lifestyles of people. UK government has developed effective policies regarding managing the weight of people in Suffolk which can assist them to prevent the prevalence of obesity.
Looking for further insights on Understanding the Prevalence of Bipolar Disorder? Click here.
Recommendation:
Reference list
Agha, M. and Agha, R., 2017. The rising prevalence of obesity: part A: impact on public health. International journal of surgery. Oncology, 2(7), p.e17.
Baker, J.F., England, B.R., Mikuls, T.R., Sayles, H., Cannon, G.W., Sauer, B.C., George, M.D., Caplan, L. and Michaud, K., 2018. Obesity, weight loss, and progression of disability in rheumatoid arthritis. Arthritis care & research, 70(12), pp.1740-1747.
Booth, H.P., Charlton, J. and Gulliford, M.C., 2017. Socioeconomic inequality in morbid obesity with body mass index more than 40 kg/m2 in the United States and England. SSM-population health, 3, pp.172-178.
Booth, H.P., Charlton, J. and Gulliford, M.C., 2017. Socioeconomic inequality in morbid obesity with body mass index more than 40 kg/m2 in the United States and England. SSM-population health, 3, pp.172-178.
Cherla, A., Renwick, M., Stefanini, G., Holmes Jr, D.R. and Mossialos, E., 2020. Cost‐Effectiveness of Cardiovascular, Obesity, and Diabetes Mellitus Drugs: Comparative Analysis of the United States and England. Journal of the American Heart Association, 9(21), p.e018281.
Croker, H., Russell, S.J., Gireesh, A., Bonham, A., Hawkes, C., Bedford, H., Michie, S. and Viner, R.M., 2020. Obesity prevention in the early years: A mapping study of national policies in England from a behavioural science perspective. Plos one, 15(9), p.e0239402.
data.england.nhs.uk, (2019), Available at:
Garcia, R., Ali, N., Guppy, A., Griffiths, M. and Randhawa, G., 2017. A comparison of antenatal classifications of ‘overweight’and ‘obesity’prevalence between white British, Indian, Pakistani and Bangladeshi pregnant women in England; analysis of retrospective data. BMC Public Health, 17(1), pp.1-7
George, M.D., Giles, J.T., Katz, P.P., England, B.R., Mikuls, T.R., Michaud, K., Ogdie‐Beatty, A.R., Ibrahim, S., Cannon, G.W., Caplan, L. and Sauer, B.C., 2017. Impact of obesity and adiposity on inflammatory markers in patients with rheumatoid arthritis. Arthritis care & research, 69(12), pp.1789-1798.
Gregg, R., Patel, A., Patel, S. and O’Connor, L., 2017. Public reaction to the UK government strategy on childhood obesity in England: A qualitative and quantitative summary of online reaction to media reports. Health Policy, 121(4), pp.450-457.
Gregg, R., Patel, S., Patel, A. and O’Connor, L., 2017. Public Reaction to the UK Government Strategy on Childhood Obesity in England. J Comm Pub Health Nurs, 3, p.176.
Hamer, M., O'Donovan, G. and Stamatakis, E., 2019. Lifestyle risk factors, obesity and infectious disease mortality in the general population: Linkage study of 97,844 adults from England and Scotland. Preventive medicine, 123, pp.65-70.\
healthysuffolk.org.uk , (2019), Available at:
Heslehurst, N., Dinsdale, S., Brandon, H., Johnston, C., Summerbell, C. and Rankin, J., 2017. Lived experiences of routine antenatal dietetic services among women with obesity: A qualitative phenomenological study. Midwifery, 49, pp.47-53.
Higgins, V., Nazroo, J. and Brown, M., 2019. Pathways to ethnic differences in obesity: The role of migration, culture and socio-economic position in the UK. SSM-population health, 7, p.100394.
Hobbs, M., Griffiths, C., Green, M.A., Jordan, H., Saunders, J., Christensen, A. and McKenna, J., 2019. Fast-food outlet availability and obesity: considering variation by age and methodological diversity in 22,889 Yorkshire Health Study participants. Spatial and spatio-temporal epidemiology, 28, pp.43-53.
Johnson, R.J., Sánchez-Lozada, L.G., Andrews, P. and Lanaspa, M.A., 2017. Perspective: a historical and scientific perspective of sugar and its relation with obesity and diabetes. Advances in Nutrition, 8(3), pp.412-422.
Keaver, L., Pérez-Ferrer, C., Jaccard, A. and Webber, L., 2020. Future trends in social inequalities in obesity in England, Wales and Scotland. Journal of Public Health, 42(1), pp.e51-e57.
Local Authority Health Profiles - PHE Available at:
Muttarak, R., 2018. Normalization of plus size and the danger of unseen overweight and obesity in England. Obesity, 26(7), pp.1125-1129.
Nobles, J., Christensen, A., Butler, M., Radley, D., Pickering, K., Saunders, J., Weir, C., Sahota, P. and Gately, P., 2019. Understanding how local authorities in England address obesity: A wider determinants of health perspective. Health Policy, 123(10), pp.998-1003.
Pinho-Gomes, A.C., Peters, S.A., Thomson, B. and Woodward, M., 2021. Sex differences in prevalence, treatment and control of cardiovascular risk factors in England. Heart, 107(6), pp.462-467.
Public Health Profiles - PHE Available at:
Viner, R.M., Kinra, S., Christie, D., Cole, T.J., Costa, S., Croker, H., Fry, T., Hsia, Y., Hudson, L., Kessel, A.S. and Morris, S., 2020. Modelling the burden of child and adolescent obesity on the health services in England. In Improving the assessment and management of obesity in UK children and adolescents: the PROMISE research programme including a RCT. NIHR Journals Library.
Welbourn, R., Hopkins, J., Dixon, J.B., Finer, N., Hughes, C., Viner, R., Wass, J. and Guidance Development Group, 2018. Commissioning guidance for weight assessment and management in adults and children with severe complex obesity. Obesity reviews, 19(1), pp.14-27.
Wilding, S., Ziauddeen, N., Smith, D., Roderick, P., Chase, D. and Alwan, N.A., 2020. Are environmental area characteristics at birth associated with overweight and obesity in school-aged children? Findings from the SLOPE (Studying Lifecourse Obesity PrEdictors) population-based cohort in the south of England. BMC medicine, 18(1), pp.1-13.
www.ons.gov.uk , (2020), Available at:
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



