Reducing Patient Waiting Time in General Practice
Introduction
This assignment aims toexplore creative approaches to lessen patients waiting time in a General Practice (GP) with the application of successful change management and leadership. Advanced access is the change proposal advocated in this report because it adopts system management techniques to provide an efficient service without increasing resources (Murray and Berwick 2003). The evidence from previous studies had discovered that patients need to wait for a consultation with a GP for a minimum period of 13 days and out of four patients, one had to wait for at least one week to get an appointment (Ansell et al., 2017). The reduction of patient waiting time in GPs is important as it leads to access to early care which lowers the chances of health deterioration due to delayed care. In addition to enhancingpatient satisfaction, as timely care with reduced waiting time leads patients to feel valued and supported for their health condition(Dahl et al. 2017). Moreover, lowering patient waiting time reduces work pressure on the health professionals caring for the large number of patients at a single time. In order to gain the benefits from reducing patient waiting time, the current change proposal has been developed. To establish the change, Kotter’s 8-step Change Management model along with the 5 Whys and “Plan, Do, Study, Act” (PDSA) cycle will be used as change management tools to explain the way the change can be executed. Furthermore, the leadership approach to be taken for the change will be discussed. For healthcare dissertation help, integrating such methods could significantly improve patient satisfaction and operational efficiency.

Background
In the NHS, 62 days of urgent GP referral has not been found to be met for cancer patients over the past 5 years. Moreover, increased delay in care is been experienced by increased number of patients (health.org.uk, 2019). The increased waiting time in the NHS, UK has led hindered management of ill-health among patients (health.org.uk, 2019). This is because early and timely care for ill-health leads individuals to get effectively treated before deterioration of their health. The increased waiting time has led patients to face increased cost of care. This is because they have to avail more complex care for their deteriorating health with increased time out of lack of timely support that could otherwise be avoided with timely health checkups (Nottingham et al. 2018).
In the UK, about a fifth of patients had to wait for an appointment to see a GP, as per the data obtained from NHS Digital (Mayor, 2018). The figure highlighted that about 42% of the appointments were consulted on the same day of the booking, 6.6% of the patients were seen within one day of the appointment and 20% were seen between 2-7 days of booking. Moreover, the time slot allotted to see a patient was only 10 minutes and 95% of the surveys showed that the time slot was too short to practice safely (Mayor, 2018). The prolonged waiting time was directly related to the greater number of patients requiring the service which exceeded the capacity of the organisation (Wise, 2018). Several approaches and models have been developed to evaluate the problems and to provide most favourable solutions to those healthcare-related problems (Paul,2012). As it was evident that with the enhanced waiting time of the patient to consult a GP, the complexity of the clinical condition of the patient might become more critical which will eventually ruin the valuable time for the treatment for the patients (de Souza, 2011).
Change Management Framework
Kotter’s 8-Step Change Management
The change management framework provides structured insight into the process to be followed for established change within an organisation (Augustssonet al. 2019). The Kotter’s 8-step Change Model informs eight key stages that are to be followed in successfully structuring and implementing a change (Mohiuddin and Mohteshamuddin, 2020). The benefit of using Kotter’s change management model is that it provides clarified description of the stages to be followed for effectively implementing the change (Teixeira et al. 2017). Thus, it is followed in making the current change as it would lead to determine effective process and structure to be followed for successful alteration in care services. As asserted by Grol and Wensing (2020), Kotter's change model is beneficial in managing change as it informs the way members involved in the change are to be prepared to work collaboratively to institutionalise the change. Thus, the model is use for the current change management as it made the leaders form collaborative work effort with effective participation of stakeholders in successful implementation of the change. As critiqued by White (2019), the limitation of using Kotter’s change model is that it leads use of increase time to be taken in implementing the change. This indicates that using the model to make the current change is going to make the leaders take more time. Another limitation is that the model is top-down and do not allow scope for co-production in implementing change (Grol and Wensing, 2020). Thus, no new ideas can be added within the change based on feedback from patients from sort-term wins in the middle for lowering patient waiting time for GP.
The first stage is creation of urgency in which the need for the identified change is communicated to people who are to participate in implementing the change. This is executed by highlighting the potential threats to be faced for not accepting the change along with the opportunities to be experienced as a result of considering and implementing the change (Teixeira et al. 2017). In this change management, at this stage, the people involved in making the change are to be made aware of the opportunities of lowering patient waiting time for care from GP such as improved care satisfaction for patients, early and timely care delivery to patients, avoiding inappropriate deterioration of patients’ health due to delayed care. Moreover, made aware of the disadvantages of not accepting the change such as patient dissatisfaction towards care, increased workload for staff and others to create a sense of urgency in acting on to establish the specific change.
The second stage is building guiding team in which leaders to make the change are to identify and the potential stakeholders required to be involved and committed in making the change are to be selected. Moreover, a powerful coalition between each team member and leader is to be created to implement the change (Balohet al. 2018). Thus, in making the determined change, at this stage, the leaders identified key stakeholders as nurses and health professional to be committed in making the change. As argued by Helfrich et al. (2017), lack of coalition between team members creates unnecessary conflict that hinders collaborative action in making change. This is because conflict is raised out of lack of trust and confusion regarding each member’s activities which makes the team for the change avoiding working together. Thus, in making the current change, the confusion and weak areas in the team are to be resolved. This is to allow them work in a collaborative manner to institutionalise the change without delaying it due to unnecessary conflict of lack of trust over one another, hindrance in sharing roles and ideas of change and others in reducing waiting times for patients in GP care.
The third stage is developing the vision and strategy for change (Mørket al. 2018). In this stage, for the current change to be implemented, the leaders are required to develop unified vision for the change. Moreover, they are to develop strategies such as online consultation, prioritisation of patients based on health context, encouraging patients to take early appointments, revamp front-line scheduling process and others that are to be implemented in making the change. This is because early appointment led to effective scheduling of patients making health professionals understand and abide by the deadline to consult with each patient, in turn, loweringwaiting times (Sun et al. 2017). Moreover, online consultation helps healthcare professionals to provide immediate assistance to potential patients at any time which lowers the chances of patient waiting time to be increased due to delayed care (Caffery et al. 2016).
The fourth stage informs that vision for change is to be communicated by the leaders to potential team members involved in making the change (Wentworth et al. 2020). As criticised by Betancourt et al. (2017), the inability to communicate vision of change to the stakeholders involved in making the change raise confusion and concern among the team regarding the goals to be achieved. Thus, in the current change management, the leaders making the change are to communicate the vision to healthcare professional and nurses so that they can have an understanding of the goals to be accomplished in successfully implementing lowering of patient waiting time through Advanced access. The communication is to be established by the leaders with the team members through use of intranet facilities and email.
The fifth stage is resolving obstacles which are to be executed by the leaders by continuously reviewing the change management activities to determine the barriers to be resolved. Moreover, the people supporting success of the change are to be rewarded to boost productivity at work in making the change (Mohiuddin and Mohteshamuddin, 2020). According to this stage, to make the current change, the leaders are to identify the probable barriers at work that are creating obstacles for the change. As stated by Lv and Zhang (2017), inability to avoid barriers in making change leads to unsuccessful endeavour of the determined alteration in services. This is because the barriers create different obstacles such as lack of resources, unnecessary delay and others for the organisation in establishing the change. Thus, probable obstacles such as presence of low staffs, hindered patient management initiative and ineffective participation in change to be faced in implementing lowering of patient waiting times are to be identified and resolved by the leaders in making the change to create a smooth and supportive environment for the stakeholders to work in making successful change.
The sixth stage is development of short-term wins where the leaders making the change are to create short-term targets to be achieved. This is to provide the individuals involved in the change to feel sense of victory and determine what further actions are to be made based on short-term targets so that the long-term change management goals can be effectively achieved (Small et al. 2016). Thus, in this change, the leaders are to create short-term targets for the healthcare professionals and nurses such as patient waiting time reduction in few community GP care to ensure long-term success of the change. The seventh stage is consolidating gains in which continuous improvement to be made in institutionalising the change with success at the end is to be determined (Haas et al. 2020). Thus, in this stage, for the current change, the leaders are required to make continuous alteration of strategic actions as required based on ongoing work progress to ensure success of the change. The eighth stage is anchoring the change in which leaders are required to develop initiative for making the established change to remain stable (Mahmood, 2018).As argued by Creberet al. (2016), ineffective monitoring of work progress after change management leads to create hindrance in implementing change. This is because the change made may not be followed appropriately after its initial implementation and without monitoring any error remains unknown, making the leaders implementing the change fail to assure its sucess. Thus, in the current change management, the leaders are required to determine the monitoring policies to be implemented so that the change of lower patient waiting time remains established.
Change Management Tools
The PDSA Cycle and 5 Whys are the change management tools to be used in implementing the determined change of lowering patient waiting time in GP practice. The PDSA cycle stands for Plan, Do, Study and Act where planning indicates assessing and developing strategies in making change (Christoff, 2018). The plan to lower patient waiting time in GPsinclude gathering patients’ information before scheduled appointment, creating policy for late arrival and non-show, design online appointments, revamp front-line schedule, and develop patient protocol. As suggested from literature, proactive healthcare workers will be considered to be the best for reducing the waiting time of the patients in healthcare organisations (Tolvanenet al. 2018). Another factor is the maintenance of the organisational charts within the healthcare organisation as this will show the vivid picture of the hierarchy and staff will be able to effectively communicate with each other in the time of a crisis as there will be no ambiguity about the functioning roles along with a proper flow of authority.
In the Do stage, the strategies plannedfor making the change is implemented (Newcombe and Fry-Bowers, 2018). Thus, in this stage for the current change management, active actions are to be taken based on the plan to alter working nature of GP to provide effective care with reduced waiting time to the patients through advanced access. The study stage informs monitoring the implementing plan for change to determine further action and alteration to be made for success of the change (Bidassieet al. 2017). Thus, at this stage, in the current change management, leaders are required to analyse the extent of success of the implemented strategies by receiving feedback from patients and healthcare professionals along with nurses. This is to determine the further alteration required for successful establishment of the change. In Act stage, the leaders are needed to implement the altered strategies based on the initial success of the plan of change (Hunt and Ojha, 2017). Thus, in this stage, the leaders are going to implement the extended change strategies for successful and effective implementation of lowering of patient waiting time in long-term condition for GP care. The benefit of using the PDSA cycle in making change is that support continuous improvement to be made in cyclic manner to ensure the determined change remains established for longer time (Mazzocatoet al. 2016). However, limitation of using PDSA cycle is that no proactive steps can be taken (Mellor et al. 2020). Thus, in the current change, by using PDSA cycle no prior indication of hindrances to create barriers for the change can be determined to develop proactive actions.
According to the 5 Whys Model, based on the first identified problem five other consecutive reasons are identified to determine the importance of making any change (Aij and Rapsaniotis, 2017). It is effective to be used in this change management, as it allowed to determine the root cause of the raised problem ensuring effective changed actions to be taken to achieve success in resolving the error or issue.
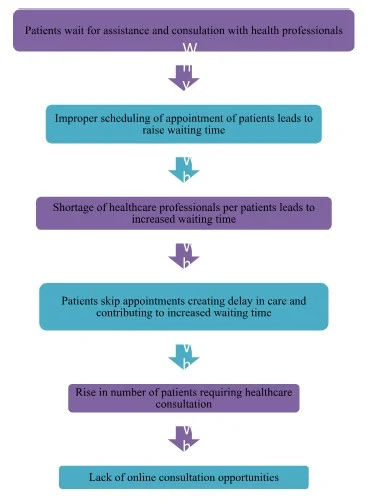
5Whys of Change Management
Leadership Approach
Leadership is considered to be an important part for targeting goals, engaging the patients andstaff, motivating staff to manage the resources and providing solutions (Avery, 2004; Northouse, 2012; Nanjundeswaraswamy et al., 2014). Among these several leadership styles, the implementation of the transformational leadership style is considered to be most effective because of the four components which include idealising influence, inspirational motivation, intellectual stimulation and individualised consideration (Northouse, 2012). In making the change, the transformational leadership is to be used at each stage. This is because this leadership allows the leaders at each stage of change to quickly analyse the situation and take effective actions with involvement from the employees to ensure growth (Asif et al. 2019). Thus, use of transformational leadership would be effective in making the determined change with effective collaboration between leaders and team members (nurses and health professionals).
Impact of proposed change on healthcare system
The proposed change of reducing waiting time for patients to get prompt GP appointment is going to impact in providing timely support and consultation to patients. This is because it would avoid delays throughout healthcare services. The current change would impact the NHS in enhancing their care quality and ensure higher satisfaction among patients while receiving care. This is because timely care with reduced waiting time will give the service users the appropriate access to care that is required for their health to prevent further deterioration as well as ensuring effective and timely intervention (Lukácset al. 2019).
Evaluation of proposed change
The evaluation of management of proposed change and its implementation is required to determine the standards of its success and consistency in improving services or problems. For evaluating the current change, the feedback from patients is to be accessed through use of close-ended questionnaire. As mentioned by James et al. (2017), patient's feedback informs to what extent they are satisfied with the current change, in turn, mentioning the extent of success of the change. Thus, feedback of patients is to be gathered regarding the extent of time reduced in waiting to be cared by GP after the change implementation to determine its success. An audit is to be conducted before and after the implementation of change to determine the extent to which waiting time with GP for consultation is reduced for the patients after the change. The increased reduction of time for waiting would indicate that the change is successfully implemented to the patients.
Way the change proposal would enhance care quality
The change that is reduction of waiting time for patients for care and consultation from GP is going to improve care quality by offering timely care support to patients who immediately require care for their deteriorated health.
Limitation of change proposal
In case of many patients, it is seen they are unable to use e-healthcare resources to control treatment and avail support (Pealing et al. 2018). In the current change proposal, it is seen that online appointment has been mentioned as one of the strategy to lower patient waiting time. However, the strategy cannot be implemented for patients who lack knowledge and skill regarding the way to use online care services in turn creating limitation towards success of the change. The other limitation to be experienced in implementing the change proposal is that the nurses may not be well-equipped and trained regarding the way to maintain effective patient protocol for visits. This would lead to create hindrance in lowering waiting times for patients in GP practice.
Ways to communicate proposed change
The stakeholders were expected to maintain an effective correspondence all through the course of action with the application of the Situation-Background-Assessment Recommendation (SBAR) Tool (NHS Improvement, 2017). This particular tool of communication will allow the staff to share the concise and highlighted information in relation to the newly implemented model. The stakeholders could discuss the strength and weakness of the newly adopted plan via the method of communication during the developmental change (Burnes, 2004). The communication about the proposed change could be done by the GP surgery website like when the change has to be implemented, what are the benefits it would provide to the service users (Greenleaf, 2002). The change implementation can also be communicated to the patients through the appointments, leaflets, through the receptionist and GP, press release (Bennett et al., 2013). All the details of the patients will be recorded in the database, therefore the author Jorgensen et al. (2008) suggested that the information can be communicated to the clients through phone calls, emails or messages with patient’s consent.
Conclusion
Lastly, it can be concluded that the several factors such as scheduling of the patients, the procedures related to the admission, the appointment time of the patient have a significant impact on the waiting time of the patient.Different studies have shown the effect of the approach on the arrival time of the patient and the service time provided. The reduction in the variables of the facilities provided significantly improves the performance. The small step by step strategies has been discussed throughout the report for the implementation of the Kotter’s Change model which will effectively reduce the patient waiting time to visit their GP. The Change proposal also focuses to provide appointments to the patients on the same day of the appointment. The report also justified the need for the change and about the effective barriers that have to be handled to ensure the change implementation.

Looking for further insights on Purchased and the nature of co ownership? Click here.
References
Aij, K.H. and Rapsaniotis, S., 2017. Leadership requirements for Lean versus servant leadership in health care: A systematic review of the literature. Journal of Healthcare Leadership, 9, p.1.
Ansell, D., Crispo, J.A., Simard, B. and Bjerre, L.M., 2017. Interventions to reduce wait times for primary care appointments: a systematic review. BMC health services research, 17(1), p.295.
Asif, M., Jameel, A., Hussain, A., Hwang, J. and Sahito, N., 2019. Linking Transformational Leadership with Nurse-Assessed Adverse Patient Outcomes and the Quality of Care: Assessing the Role of Job Satisfaction and Structural Empowerment. International journal of environmental research and public health, 16(13), p.2381.
Augustsson, H., Churruca, K. and Braithwaite, J., 2019. Mapping the use of soft systems methodology for change management in healthcare: a scoping review protocol. BMJ open, 9(4), p.e026028.
Baloh, J., Zhu, X. and Ward, M.M., 2018. Implementing team huddles in small rural hospitals: How does the Kotter model of change apply?. Journal of nursing management, 26(5), pp.571-578.
Bennett, J.L. and Bush, M.W. 2013. Coaching for change. Routledge.
Betancourt, J.R., Tan-McGrory, A., Kenst, K.S., Phan, T.H. and Lopez, L., 2017. Organizational change management for health equity: perspectives from the disparities leadership program. Health Affairs, 36(6), pp.1095-1101.
Bidassie, B., Gunnar, W., Starr, L., Van Buskirk, G., Warner, L.J. and Anckaitis, C., 2017. A modified collaborative model to improve surgical flow health care processes in Veterans Affairs Medical Centers. International Journal of Healthcare, 3(2), pp.47-56.
Burnes, B. 2004. Kurt Lewin and the planned approach to change: a re‐appraisal. Journal of Management studies, 41(6), pp.977-1002.
Caffery, L.J., Farjian, M. and Smith, A.C., 2016. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: A scoping review. Journal of telemedicine and telecare, 22(8), pp.504-512.
Christoff, P., 2018. Running PDSA cycles. Current problems in pediatric and adolescent health care, 48(8), pp.198-201.
Creber, R.M.M., Maurer, M.S., Reading, M., Hiraldo, G., Hickey, K.T. and Iribarren, S., 2016. Review and analysis of existing mobile phone apps to support heart failure symptom monitoring and self-care management using the Mobile Application Rating Scale (MARS). JMIR mHealth and uHealth, 4(2), p.e74.
Dahl, T.L., Vedsted, P. and Jensen, H., 2017. The effect of standardised cancer pathways on Danish cancer patients' dissatisfaction with waiting time. Dan Med J, 64(1), p.A5322.
de Souza, L.B. and Pidd, M., 2011. Exploring the barriers to lean health care implementation. Public Money & Management, 31(1), pp.59-66.
Greenleaf, R.K. 2002. Servant leadership: A journey into the nature of legitimate power and greatness. Paulist Press.
Grol, R. and Wensing, M., 2020. Effective implementation of change in healthcare: a systematic approach. Improving Patient Care: The implementation of change in health care, pp.45-71.
Haas, M.R., Munzer, B.W., Santen, S.A., Hopson, L.R., Haas, N.L., Overbeek, D., Peterson, W.J., Cranford, J.A. and Huang, R.D., 2020. # DidacticsRevolution: Applying Kotter’s 8-Step Change Management Model to Residency Didactics. Western Journal of Emergency Medicine, 21(1), p.65.
health.org.uk 2019, NHS performance and waiting times, Available at: https://www.health.org.uk/news-and-comment/blogs/nhs-performance-and-waiting-times [Accessed on: 10 July 2020]
Helfrich, C.D., Simonetti, J.A., Clinton, W.L., Wood, G.B., Taylor, L., Schectman, G., Stark, R., Rubenstein, L.V., Fihn, S.D. and Nelson, K.M., 2017. The association of team-specific workload and staffing with odds of burnout among VA primary care team members. Journal of general internal medicine, 32(7), pp.760-766.
Hunt, R.J. and Ojha, D., 2017. Oral health care quality measurement and its role in dental education. Journal of Dental Education, 81(12), pp.1395-1404.
James, T.L., Calderon, E.D.V. and Cook, D.F., 2017. Exploring patient perceptions of healthcare service quality through analysis of unstructured feedback. Expert Systems with Applications, 71, pp.479-492.
James, T.L., Calderon, E.D.V. and Cook, D.F., 2017. Exploring patient perceptions of healthcare service quality through analysis of unstructured feedback. Expert Systems with Applications, 71, pp.479-492.
Lukács, G., Kovács, Á., Csanádi, M., Moizs, M., Repa, I., Kaló, Z., Vokó, Z. and Pitter, J.G., 2019. Benefits Of Timely Care In Pancreatic Cancer: A Systematic Review To Navigate Through The Contradictory Evidence. Cancer Management and Research, 11, p.9849.
Lv, C.M. and Zhang, L., 2017. How can collective leadership influence the implementation of change in health care?. Chinese Nursing Research, 4(4), pp.182-185.
Mahmood, T., 2018. What models of change can be used to implement change in postgraduate medical education?. Advances in medical education and practice, 9, p.175.
Mayor, S. 2018. New NHS app will let patients book GP appointments on mobiles.Allan, K. (2001). Communication and consultation. York: Joseph Rowntree Foundation.
Mazzocato, P., Stenfors-Hayes, T., von Thiele Schwarz, U., Hasson, H. and Nyström, M.E., 2016. Kaizen practice in healthcare: a qualitative analysis of hospital employees' suggestions for improvement. BMJ open, 6(7).pp.34-56.
Mellor, C., Blackman, J., Barker, E., Bhula, Z., Sibanda, E., Rawlings, E., Harrington, D. and Combe, G., 2020. Wellbeing Wednesdays: nurse-led clinic for improving physical health care in a general adolescent inpatient unit. British Journal of Nursing, 29(4), pp.230-235.
Mohiuddin, S. and Mohteshamuddin, K., 2020. Combination model for sustainable change by utilizing the Kotter's change model and the Hersey & Blanchard's leadership model for improving medication errors reporting. Journal of Medical & Allied Sciences, 10(1), pp.25-32.
Mørk, A., Krupp, A., Hankwitz, J. and Malec, A., 2018. Using Kotter's change framework to implement and sustain multiple complementary ICU initiatives. Journal of Nursing Care Quality, 33(1), pp.38-45.
Murray, M. and Berwick, D.M (2003) Advanced access. Reducing waiting and delays in primary care. JAMA, 289, p.1035-1040.
Newcombe, J. and Fry-Bowers, E., 2018. Improving postoperative neonatal nutritional practices in an intensive care unit using the PDSA cycle. Journal of Pediatric Health Care, 32(5), pp.426-434.
Nottingham, Q.J., Johnson, D.M. and Russell, R.S., 2018. The effect of waiting time on patient perceptions of care quality. Quality Management Journal, 25(1), pp.32-45
Paul, J.A. and Lin, L., 2012. Models for improving patient throughput and waiting at hospital emergency departments. The Journal of emergency medicine, 43(6), pp.1119-1126.
Pealing, L., Tempest, H.V., Howick, J. and Dambha-Miller, H., 2018. Technology: a help or hindrance to empathic healthcare?. Journal of the Royal Society of Medicine, 111(11), pp.390-393.
Rafiq, M. and Ahmed, P.K. (2000). Advances in the internal marketing concept: definition,
Small, A., Gist, D., Souza, D., Dalton, J., Magny-Normilus, C. and David, D., 2016. Using Kotter's change model for implementing bedside handoff: a quality improvement project. Journal of nursing care quality, 31(4), pp.304-309.
Sun, J., Lin, Q., Zhao, P., Zhang, Q., Xu, K., Chen, H., Hu, C.J., Stuntz, M., Li, H. and Liu, Y., 2017. Reducing waiting time and raising outpatient satisfaction in a Chinese public tertiary general hospital-an interrupted time series study. BMC Public Health, 17(1), p.668.
Teixeira, B., Gregory, P.A. and Austin, Z., 2017. How are pharmacists in Ontario adapting to practice change? Results of a qualitative analysis using Kotter’s change management model. Canadian Pharmacists Journal/Revue des Pharmaciens du Canada, 150(3), pp.198-205.
Wentworth, D.K., Behson, S.J. and Kelley, C.L., 2020. Implementing a new student evaluation of teaching system using the Kotter change model. Studies in Higher Education, 45(3), pp.511-523.
White, K.M., 2019. Change theory and models: Framework for translation. Translation of Evidence Into Nursing and Healthcare, p.60.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



