Childhood Supracondylar Fracture Analysis
1.0 Introduction
As part of the PGD clinical reporting in the appendicular and axial skeleton program, it is a requirement to develop a case study following a shadowing of a patient involved in a minor injury. This case study relates to supracondylar fracture of the distal humerus in children. It will illustrate in detail the types of injury and its classification and the management of the patient from check-in time to the accident and emergency department to discharge post-treatment. Furthermore, it will also focus how the diagnostic examination is important in patient clinical management as well as in the interprofessional practice in this setting. The ideal trauma patient for this case needed to have been involved in a traumatic injury and for whom a radiographic examination was necessary as part of their patient management plan. Permissions from the patient and parents were sought, and the purpose of this study was explained to the parents and the patient. A six years old boy was brought to the paediatric emergency department by his parents after he had fallen off the monkey bar onto hyperextended arm at the playground. The patient was admitted in Accident and Emergency 1 hour after trauma. He had a free fall and landed on a soft sandy area and did not injure his head. At the time of the injury and after the injury the patient was awake and did not lose consciousness. The patient’s initial complaint was pain and reduced range of movement of his left dominant arm. No other previous medical condition was reported. The signs and symptoms were bruising over the elbow, severe pain in the elbow and forearm, swelling around the elbow joint and the proximal forearm. The patient has also been unable to move or straighten the arm.
Looking for further insights on Childhood? Click here.
1.2 Clinical History
The clinical condition relates to the signs and symptoms - Painful and swollen elbow with minimal posterior prominence deformity of the elbow. The affected arm appeared slightly shorter than the other arm. The patient had presented with normal temperature (37 Celsius) and blood pressure (105/65). There were neither evidences of open wound nor obvious puckering of the skin clinically. Upon palpation of the entire limb, there was no suspicion for any other fracture or dislocation hence no differential diagnosis. Clinical examination ruled out no neurovascular compromise; the radial pulse was present – Capillary refill time was normal with warm pink hand indicating good circulation. Neurological examination of the three major nerves (median, radial and ulnar) was unremarkable. All the results of the clinical diagnosis led to a suspicion of distal humerus supracondylar fracture. In a study conducted by Leaman, Hennrikus and Bresnahan (2016) on identifying non-accidental injury in children under the age of 2; out of 115 patients presented in their emergency department and paediatric clinic, 19 of them were reported as non-accidental injury related. They have also looked at numerous studies in relation to supracondylar humerus fracture in non-accidental injury and found only 0.5% of involvement. Although this figure appears to be very low, it is Important that the clinician obtain a full history regarding the fracture to differentiate accident and non-accident injury in the supracondylar humerus fracture as illustrated by National Institute for Health and Care Excellence (NICE 2016). When examining a child involved in trauma with elbow pain, the clinician should ensure that the entire limb is assessed; this is because secondary fracture may be present (Kumar and Singh, 2016). The latter situation can further complicate the clinical management of the patient if suspected. The clinician should also evaluate for neurovascular and soft tissue involvement to free from the risk of compartment syndrome, neurovascular damage, Volkmann’s ischaemic contracture and malunion (Naik et al., 2017). Clinical tests for supracondylar fracture include capillary refill test, radial pulse and neurovascular examination of the three nerves namely radial, ulnar and median and in doing so, the standard trauma survey should be followed (Wolf et al., 2013). Nonetheless, the Absence of pulse in a supracondylar fracture in children is an indication for brachial artery damage even if the hand is presented with warm pink appearance (Usman, Jamil, and Hashmi, 2017).

A study conducted by Usman, Jamil and Hashmi., (2017) assessed the management of vascular injury involved with a supracondylar fracture of the humerus with pulseless hand and concluded that immediate vascular exploration is must for a cold, pulseless hand. Moreover, the study recommends early vascular investigation even for the pulseless warm pink hand; this is to avoid further complication. In their study 82 % of the patient were males, and 18% were female; this is a good indication of the predominance of the male group in this kind of injury. Besides 72.7% off the injury were left-sided and 27.3% of the injuries were right sided, this figure matches with the common agreement of the non-dominant side of the limb associated with supracondylar fracture. The second primary concern in garland type 3 classification of supracondylar fracture of the distal humerus is the potential injury to all the three major nerves and the brachial artery. More specifically the ulnar nerve is more prone to damage as it naturally originates from the posterior side of the elbow and links the medial epicondyle and trapped in between the bone and the superficial skin. According to Leiblein et al. (2017), vascular complications encountered in garland type 3 and flexion type supracondylar fracture ranges from 3.2 to 14.3 %. On the same note, Leiblein et al., (2017) reported that nerve involvement in the supracondylar fracture is between 12 to 20 %. Therefore, it is very important that the clinician diagnose the patient properly to avoid orthopaedic pitfalls (Kumar and Singh 2016).
1.3 Epidemiology - Supracondylar Fracture of the Distal Humerus
Supracondylar fractures of the distal humerus are fractures involving the lower end of the humerus, and its fracture line runs above the line joining the medial epicondyle and the lateral epicondyle subsequently above the insertion of the supinator muscle (Timothy et al., 2016). Therefore, it is an extra-articular metaphyseal fracture. There are two types of supracondylar fractures extension and flexion, the extension type being the most common type of fracture (Verka et al., 2017). Complications attached to this kind of fractures can lead to surgical intervention due to vascular injuries, polytrauma and open and comminuted fractures (Wolf et al., 2013). Also, these fractures occur due to the high energy of traumatic injury. All in all, the treatment for the supracondylar fracture depends upon the extent and the severity of the fracture (Verka et al., 2017). Nonetheless, the ultimate treatment is to reduce and mobilise the fracture under closed or open reduction technique. Fracture of the distal humerus in children is very frequent, and it represents 60% of all paediatric elbow fractures and 16% of all paediatric fractures as per (Kumar and Singh, 2016). Moreover, Kumar and Singh (2016) reports that the age group between 5-7 years are the most affected ones. However, their study does not mention the reason why this age group is the most presented. However, Verka et al. (2017) suggested that this frequency in this age group is due to the weakest part of the metaphyseal area of the distal humerus involvement and fault the increased ligamentous laxity for this occurrence. Noteworthy, available literature reveals that both boys and the non-dominant side are highly at risk of these fractures.
Supracondylar fracture of the distal humerus in children is different from the adult for the following reasons:
• Bones are still in a growth phase • Have higher remodelling capability • Secondary ossification centres make the radiographic appearance very different in contrast to adult (Kim and Gauguet, 2018).
There are six ossification centres within the paediatric elbow joint, out of which 4 of them are located on the humerus. The other remaining two are located inferiorly to the humerus namely the epiphysis of the radial head and the apophysis of the olecranon. At birth, the humeral epiphysis is entirely cartilaginous. The ossification centres at the elbow get ossified and fused with the adjacent bone as the children get older. It is also important to note that the ossification centres appear by order as the age progress. The first ossification centre to appear at the age of approximately one year is the capitulum then at around three the radial head then around five years medial epicondyle then around seven years the trochlea after that at the age of nine the olecranon and finally the lateral epicondyle at the age of eleven. This sequence of appearance is also known by the mnemonic C-R-I-T-O-L. It is estimated that the complete ossification in girls is achieved at the age of 6 to 8 and for boys at the age of 8-12. Numerous studies and books widely accept these figures and order of appearances (Kim and Gauguet, 2018)
1.4 Justification for Examination
Upon proper clinical examination clinicians request radiograph to evaluate fracture anatomy, the severity of the fracture and its classification, the exact location of the fracture, soft tissue involvement, effusion, degree of displacement and angulation. This information is important for the treatment plan and patient management (Nayak et al., 2013). Radiographic examination sometime reveals incidental findings such as benign and malignant tumours (Andrade -Neto et al., 2016). Also, associated injuries are a major concern in traumatic injury. Therefore, the adjacent painful area may be requested for an x-ray (Kumar and Singh 2016). According to United Nations Scientific Committee on the Effects of Atomic Radiation (Del Rosario Perez, 2014), the use of ionising radiation to treat and diagnose human pathologies has augmented globally. Although modern safety applications and technology have enormously eliminated the risk of accidental risk of radiation to patient and staff, there are still greater risks associated with ionising radiation due to carelessness and poor clinical diagnosis leading unnecessary radiation exposure (Del Rosario Pérez, 2014). According to literature by Del Rosario Pérez (2014) numerous radiological examination procedures may be unfitting (>20% in certain cases). To avoid unnecessary exposure to radiation and to obtain optimal results; justification for radiological examination should take in consideration all the scientific pieces of evidence such as the laboratory tests results, clinical information, history, previous medical imaging reports and on top of all the later, a thorough professional evaluation should take place prior to ordering for radiological examination (Del Rosario Pérez, 2014). This is because numerous studies have faulted healthcare professionals lacking cognizance of radiation doses and associated risk for an unnecessary demand of radiological examination (Shiralkar et al., 2003; Lee et al., 2004; Del Rosario Pérez, 2014). To straighten the measures regarding radiation protection worldwide and to prevent unnecessary use of ionising radiation; the International Commission of Radiation Protection (ICRP) has set up recommendations for radiation protection; these recommendations advocate justification, quality control, optimal use, adequate training.
Radiographic Examination and Its Relevance in Patient Management
On lateral X-ray, there is an obvious anterior cortical break demonstrated at the distal humerus. The anterior humeral line does not intersect the capitellum while the posterior cortex is intact. On the AP view, a longitudinal fracture line can be seen at the distal shaft of the humerus, and a dense sclerotic area adjacent to the olecranon fossa suggesting of impaction also can be observed. Posterior and elevated anterior fat pad could also be seen with marked soft tissue swelling. Upon discussion with the referring clinician, it was agreed that there was a posteriorly displaced supracondylar fracture of the humerus. The classification for this type of injury is Gartland type 2 fractures. It is important to note that radiographic examination (see figure 1) plays a vital role in orthopedic. Diagnosis of any bony injury is first clinically investigated using physical examination and other diagnostic tests and finally the radiographic examination request to confirm the clinical findings. This practice is implemented to avoid an unnecessary exposure to ionising radiation (IRMER 2017).

Moreover, radiographic examination is very relevant in the patient management; this is because radiograph provides vital information regarding the severity of the fracture and the classification of the fracture. Therefore, it plays a vital role in the patient management and decision making towards the treatment (NICE, 2016). Ideally, Radiographic lines such as the anterior humeral line and the Baumann’s angle (as illustrated in the figures below) are used to determine the angle and the displacement in supracondylar humerus fracture (Alton, Werner, and Gee, 2014).
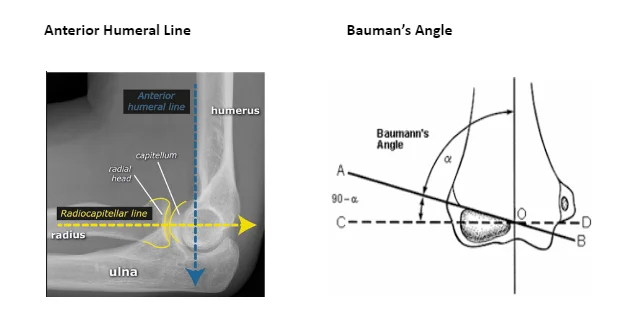
The radiographic examination begins with a lateral view of the distal part of the humerus and an Antero-Posterior (AP) View albeit Standard AP view may not be possible all the time especially with severely displaced and comminuted fractures; this is due to restricted movement and pain (Kumar and Singh, 2016). Radiographer should always be vigilant of not aggravating the condition by moving or asking to move the affected limb to achieve textbook style radiograph. In a severely displaced fracture, one initial view is recommended by Thornton and Gyll (1999) to avoid nerves or artery damage. Likewise, the non-displaced and occult fracture may not always reveal obvious radiographic evidence of fracture except for the sign of posterior and anterior elevated fat pad (Kumar and Singh 2016). Baumann angle is used to evaluate the carrying angle thus evaluate the cubitus varus deformity. The angle is obtained by intersecting a vertical line along the axis of the humerus and a line along the growth plate of the lateral epicondyle. According to Biradar and Khan (2017), the normal angle is between 70 and 74 degrees. Moreover, for every 5-degree variation in Baumann angle, there is a 2-degree change in carrying angle (Biradar and Khan, 2017). Biradar and Khan (2017) studied the accuracy of Baumann's angle by comparing and assessing the Baumann angle and the carrying angle of the uninjured side with the affected side post satisfactory reduction. The ultimate aim of the study was to predict how reliable the Baumann angle is to diminish the incidence of cubitus varus in supracondylar fracture of the distal humerus. They concluded that the Baumann angle is useful and reliable. When analysing the methods of the study, it is important to point out that the number (28) of the patient included in the study is very small. Besides regarding the demographic characteristic, out of the 28 selected patients in this study, 18 of them were male, keeping in mind that all the 28 patients in this study were treated in the same hospital. This selection bias is a potential concern. The authors mentioned in the method that they used an improvised goniometer to measure the carrying angle but no specific information was given on how this improvised instruments had been used in this study. Nonetheless, a Major drawback of this study is failing to inform how the improvised tool was used in this study. This situation can be rectified by being more informative.
1.5 Radiographic report of the subject in this study

Whereas the radiographic reports identify the posterior displacement, it does not identify comminution. Similarly, the final report does not acknowledge the distal humerus and and the anatomical side of the limb. Instead, it states about “supracondylar fracture”. Nonetheless, this has minimal impact on the patient because when the clinician finally receives the report, they will receive information on the specific name of the patient together with the anatomical side of the limb. Noteworthy, this is not a good standard of practice because all reports must give information on the subject body part.
1.6 Classification
There are two types of supracondylar fracture namely the extension and flexion type fractures. According to Kim and Gauguet (2018), 95% of the distal humerus supracondylar fractures are extension type fractures, and the other five per cent are flexion type fracture. Extension type fracture usually occurs when there a fully extended elbow falls on an outstretched hand (Leiblein et al. 2017). This occurrence is mainly due to the weakest part of the metaphyseal area of the distal humerus, associated with the presence of olecranon fossa in the posterior plane and coronoid fossa in the anterior plane making it a high risk for fracture. On the other hand, Flexion type fracture occurs due to falling directly on a flexed elbow. As a result, the distal fragment is displaced anteriorly (Carrazzone et al. 2017) Extension type fractures being the most common type, they are further classified based upon Gartland classification. Studies show that the Gartland classification is the most useful classification in this category (Naik et al., 2017). This classification represents the three stages of the distal fracture fragment displacement in relation to the proximal humerus: the first type being a non-displaced fracture or minimally displaced fracture, the second type is an incomplete fracture associated with posteriorly displaced fracture and with intact posterior cortex while the third type is a completely displaced fracture associated with anterior and posterior cortical disruption, thus making it unstable in extension and flexion. Unlike in the flexion type fracture, in the extension type fracture, the posterior periosteum remains undamaged and as a result it provides stability and facilitates the reduction. The classification dictates the method of treatment and helps to identify problems encountered concerning prognosis and complications. It also provide vital information regarding the structure of the fracture (Alton, Werner, and Gee, 2014) Gartland classification was further studied and modified by Wilkins KE in 1984 (Alton, Werner, and Gee, 2014) and as illustrated further in appendix 1, the following are the classifications:
These modifications add the following subtypes:
• Type 2A Gartland classification which refers to extended fracture without rotation. • Type 2 B Gartland classification comes with some degree of rotation • Type 3A Gartland classification refers to intact medial periosteal hinge with distal fragment displaced posteromedial. Type 3B applies to intact lateral periosteal hinge with the distal fragment displaced posterolaterally. • Type 4 Gartland classification was suggested by Leitch and his colleagues in 2006 (Alton, Werner, and Gee, 2014) this study will only Focus on the garden classification.
Type 1 Gartland classification fracture is a stable fracture without angulation or with minimal angulation within the acceptable limit. The anterior humeral line determines the acceptability of the angulation limit on the lateral elbow X-ray. This line should intersect at least a third of the capitulum. Other indicators are elevated anterior fat pad and posterior fat pad seen on the lateral X-ray. They are very stable fractures because they are characterised by intact periosteum (Leiblein et al. 2017). Nonetheless, according to Gartland (1959), physicians should not expect any evidence of vascular or nerve compromise. Type 2 Gartland classification fracture is also a stable fracture with reasonable cortical integrity. The posterior cortex undergoes minimal damage; however, it maintains the length. The apparent deformity of this fracture is the angulation. And the integrity of the cortex should prevent rotation. On the X-ray, in this case, the middle third of the capitulum is not intersected by the anterior humeral line (Naik et al., 2017). According to Alton, Werner, and Gee (2014), Type 3 Gartland classification fracture is a displaced supracondylar fracture without significant cortical contact. Generally, there is an extension in the sagittal plane and rotation in the frontal or transverse plane. In most cases, the periosteum is extensively torn, and this fracture usually causes damage to the soft tissue and vascular injury.
2.0 Role of diagnostic examination in the clinical management of the patient in the context of interprofessional practice
Diagnostic examination is about information gathering and integration and interpretation of patient’s condition or disease. interprofessional practice refer to teamwork, interprofessional care, and the main objective is to provide quality care for the patient and cure the disease quickly (Nancarrow et al., 2013). An interruption in the interprofessional collaboration work cycle for example if a false negative or a false positive result encountered due to human error or carelessness and this will result in errors and discrepancies. Therefore, delay for treatment and potential harm for the patient subsequently affect patient management (Madani et al., 2018). The selection of appropriate diagnostic examination and the knowledge behind producing good standard diagnostic images are important in terms of effective patient management (Sor.org, 2012). The timely manner reporting and accurate interpretation are fundamental for effective clinical management of the patients (Sor.org, 2012). For example, a good team having shared goals and accountability in the radiology department will produce quality and timely imaging service thereby providing better service to the referring clinicians and in return, the clinician will be able to better serve the patient. (Larson et al., 2014) Therefore, interprofessional practice is a key factor in any organization more specifically in a healthcare setting. Accurate communication, good quality, and timely examination will lead to a fast-clinical decision-making thereby rapid treatment for the patient better health outcome and positive results for the trust (Larson et al., 2014). Literature by Nancarrow et al. (2013) stated that the result of the teamwork has a potential impact on quality of care, staff satisfaction, and staff motivation, and concluded that the teamwork outcome is interconnected with the organisation, healthcare professionals and the patient.
3.0 Relationship of the radiographic report to others diagnostic tests relating to collaborative working
Radiology reports are influenced by clinical details which includes other test results such as physical tests and laboratory test. But, radiography examination is only one section of the entire medical diagnosis process of the patient. Against this background, It is mostly used to confirm a clinical finding and therefore, they are very much interconnected in the process of diagnosis. Like any other tests results, radiology reports are also susceptible to errors and discrepancies. They cannot be 100 % accurate in most cases (Bruno et al., 2015). On this note, Niazkhani, Bal and Pirnejad, (2013) reveal studies which identified that the most common error in diagnostic radiology and allegation on radiologist were due to poor communication information such as clinical details and other results. Niazkhani, Bal & Pirnejad (2013), cites a study which identified that in a major teaching hospital in Sidney, almost half of the incident relating to the radiology was due to an interruption in communication. Communication among healthcare professionals is crucial; especially the clinical information containing other test results supplied by the referring clinician to the radiologist must be accurate to obtain a good report from the radiologist. Any interruption or misrepresentation in the normal communication of this important information can lead to a delay in treatment and inaccurate diagnosis (Niazkhani, Bal and Pirnejad, 2013).
4.0 Recommendation related to the suitable form of management of the patient
NICE (2016) guidelines on non-complex fractures stipulate adequate and updated training for all healthcare professionals in the trauma service. This will improve patient management. Worldwide, emergency departments are facing the increased flow of patient and challenges (Jarvis, 2016). To achieve high patient satisfaction and rapid patient diagnosis, hospitals need to make sure that the staff level is maintained and that patient is seen quickly so that they don’t occupy the beds longer than required and delay the entire system (Jarvis, 2016). Jarvis, (2016) has identified in his study numerous features such as doctor triage, rapid assessment model, streaming process, the point of care testing as strong factors promoting rapid diagnosis and reduced waiting time in the emergency departments - and as a result, better patient management and satisfaction. Introduction of these features should be considered nationwide to promote better patient management. Niazkhani, Bal and Pirnejad, (2013) have identified in their study that having cutting-edge Radiology Information System within the radiology department will eliminate any error in feeding patient details as well as clinical information versus the paper version of requesting radiology examination. They also identified that having such system encourages the direct communication with the clinician and radiologist whereas when doing on paper format, information might get misinterpreted by nurses who something requests radiographic examination on behalf of the clinician.

5.0 Treatment
Treatment for supracondylar fracture of the humerus depends upon the severity and the displacement of the fracture (Kumar and Singh, 2016). Ideally, non-displaced fracture (type 1 garland classification) is generally treated with above elbow splint immobilisation in 90 degrees for 3 weeks (Kumar and Singh, 2016). According to literature by Kumar and Singh (2016), constricted casting and excessive flexion is a risk of compartment syndrome, therefore, should not be practiced. However, if more than 10 degrees of the virus is depicted at the fracture site, open reduction fixation is desirable (Kumar and Singh, 2016). Treatment for garland type 2 fractures is very controversial in regards to how it should be managed, the common agreement is to do close reduction and cast. However, most recent studies advocate close reduction with pinning (Mostafa, 2017). Kumar and Singh (2016) also highlight studies which demonstrated that the use closed reduction along with pinning in garland type 2 fractures is very satisfactory in comparison with closed reduction alone without pinning. Treatment for garland type 3 fractures come with a variety of complications and options as there are susceptible to neurovascular involvement (Kumar and Singh, 2016). The standard management is closed percutaneous pinning, but open reduction might be used when closed reduction not feasible due to the rotation and severe displacement of the fractured fragments (Li et al., 2017). As illustrated further in appendix 2, options of pins configuration are the following:
• Medial to lateral (cross pins) pins considered to be safer and more stable concept by several studies but has its disadvantages of potential ulnar nerve damage (Naik et al., 2017); • 2 lateral pins configurations will avoid the ulnar nerve damage but reported by several studies to be unstable and prone for alignment (Pavone et al., 2016). • 3 lateral pinning is also in use and been widely accepted as a good pin configuration type (Dekker, Krijnen and Schipper, 2016)
References
- Gartland J. (1959) Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet; 109:145–154.
- Thornton A. & Gyll C. (1999) Children's fractures. London [u.a.]: Saunders.
- Timothy W. et al. (2016) McRae's Orthopaedic Trauma and Emergency Fracture Management. London: Elsevier. Third Edition
- Zhong W., & Wang W. (2016) Original article: Clinical study of emergency treatment and selective closed reduction for the treatment of supracondylar humerus fracture in children, Journal of Acute Disease, 5, pp. 466–469. doi: 10.1016/j.joad.2016.07.002.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



