Enhancing Nurse Communication in End-of-Life Care
Introduction
The nursing care is provided and supervised by the registered nurses that are important as they through the use of their specialised skills and training offer appropriate care to treat physical and emotional alignments and needs of the patients. This is to ensure improved quality health of the patients and their speedy recovery (Doenges et al. 2019). In end-of-life care, effective contribution from the nurses is required to offer effective treatment so that the physical, social, emotional and spiritual needs of the patients, as well as their families, are resolved (Noome et al. 2016). The nurses in end-of-life care have the key goal to control different pain and other distressing symptoms among the patients. The end-of-life care includes supportive care, palliative care and hospice care (Kinley et al. 2018). The nurses in the end-of-life care delivery have to establish effective communication so that the needs and demands of the patients are understood and care service information required by the families of the patients to develop acceptance towards their family member's condition can be built (Masaki et al. 2017). Thus, in this study, the key aim is to determine whether or not effective educational programs is able to improve nurses communication skill that is intended for supporting the patient and their family during the end-of-life condition.
Background of the study
The end-of-life care is referred to the nature of care which is provided to the patients who are near to the end-of-life condition and have avoiding to accept proper treatment or cure for controlling their health complications (Bennett, 2016). In the UK, in 2016 nearly 46.9% deaths of patients are reported to occur within the hospital, whereas 23.5% deaths to have occurred within the own homes of the patients and 5.7% deaths occurred in the hospice care (gov.uk, 2018). This indicates that majority of the deaths of the patients who are in their end-of-life condition are occurring within the hospital and care home environment where the nurses are in charge of caring of the patients. In the study of Banerjee et al. (2016), it is mentioned that nurses in hospitals and care homes are facing hindrance in establishing effective communication with the patients and their family members regarding end-of-life care which is making them deliver false hope of life to the patients. It is leading patients and their family think of experiencing unrealistic positive outcome expectations which are not later fulfilled leading to create issues of distorted perception of the family members towards the care efficiency of the nurses.

The nurses mentioned that due to lack of knowledge regarding the way to develop communication in end-of-life care is leading them to develop issues of supporting the patients. This is because ineffective interaction by the nurses is making them unable to determine the specific needs and demands of the patients, in turn, leading them to deliver care that is not satisfactory for the patients (Gillett et al. 2016). Thus, the ineffective and unsatisfactory care received from the nurses in end-of-life condition by the patients through establishment of improper communication is creating issues of poor care for the patients and false hope among the families. As mentioned by Brooks et al. (2017), the inability to develop effective communication by the nurses in end-of-life care has become an issue as they are facing problems for proper prognosis of the patient’s condition. This is because hindered communication is leading nurses to determine the exact symptoms and detailed health reports of the patients making them unable to understand the nature of health issues being faced by the patients. As argued by Montgomery et al. (2017), hindered communication establishment by the nurses in end-of-life care is a problem as it is making the nurses deliver unclear care directives to the patients. This is because hindered interaction is leading the nurses to directly communicate with the patients about the activities they are to follow in supporting effective access care from the nurses.
The improper nursing communication skills in end-of-life care is a problem as it is making nurses develop collaborative decision by discussion with the patients regarding the nature of care to be provided to them. It is leading to create lack of competence from the patients as they are not showing inclination to accept the care (Travers and Taylor, 2016). In the study Fosse et al. (2017), the lack of effective communication skills among the nurses in end-of-life care has been regarded as an issue because it is leading the nurses to develop poor communication with the families of the patients. This, in turn, is affecting the nurses to be unable to develop proper support and approval of the nature of care from the families determined to be effective for the patient in the condition to enhance their health. Moreover, the improper communication establishment by the nurses in end-of-life care has affected them to be incapable of creating a proper environment to discuss the end-of-life condition of the patient to their families. This has led the families to show greater emotional turmoil and acceptance of the death of the patient at the end of care (Mani, 2016).
The improper communication skill among the nurses in end-of-life care has currently become an issue because it is creating hindrance to show support towards the cultural differences and spiritual needs of the patients (Omar Daw Hussin et al. 2018). This is because without effective establishment of interaction the nurses are unable to determine the cultural and spiritual preferences of the patients, in turn, making them show lack of compliance in accepting care. In addition, the improper communication establishment by the nurses in end-of-life care is creating issues for them to inform clearly to the families and patients the difference between natural death or the extreme and futile measures to be used in supporting the condition of the patient in the end-of-life days (Isaacson and Minton, 2018). The hindered communication skill in end-of-life has currently created issues among the nurses to be incapable to educate the families regarding the need of technology to be used to keep the patient living. This has led nurses in end-of-life care to develop- conflict with the families of the patients to deliver care (Threapleton et al. 2017). Thus, in this study, the discussion regarding the impact of educational programs on the communication skills of the nurses for supporting patients and their family members in end-of-life care is to be discussed. This is to ensure whether or not the programs are effective to resolve the issues and improve communication skills of the nurses in end-of-life care as it is one of the essential aspects to be successful to deliver quality support to the patients and their family members.
Literature Search
Search Strategy
The search strategy indicates the way search terms are to be used for identifying required information through the use of search tools and databases. In order to search and analyse literature, the study is going to use the systematic literature review process as the search strategy. The systematic literature review is referred to the process in which systematic methods are used for collecting secondary information through critical analysis of relevant research studies and synthesising findings that are quantitative or qualitative in nature (Chang and Lin, 2016). Thus the systematic review is designed in such a way that it provides complete and exhaustive summarization of evidence that are comprehensive, transparent, replicable and methodical. The systematic review is to be used in the study because it allows the researcher towards findings information in an unbiased form ensuring the development of the stud in a reliable and accurate manner (Evripidou et al. 2019). Thus, the use of the method is going to allow development of enriched study with potential information. The systematic review develops summarization of data by exploring multiple studies which makes it easier for the researcher to gather wide amount of data regarding the research topic from different perspectives presented in the study. Moreover, the systematic review is beneficial as it allows developing idea regarding the way the findings can be applied in everyday practise along with is cost-effective in nature (Richards et al. 2018). Thus, the systematic review method is to be used as it would allow enriched information to be collected without much expenditure and in less time.
Database used
The electronic search databases are to be used in the study for collecting updated and relevant studies regarding the search topic. The electronic search databases are referred to the ones which have organised collection of data regarding different search topics that are stored electronically to be accessed by researcher (Jarden et al. 2020). This nature of databases is to be used because it allows researching relevant and current evidence regarding the topic of interest with effective use of specific search words. Moreover, use of electronic search databases for researching information is essential in the study as it is going to allow the researcher develop easier findings of data within less time in comparison to search information collected from books and journals. The electronic search database platforms to be used in the study include Medline, PubMed, Google Scholar, CINHAL and others.
Search Terms
The identification of specific search term regarding the research topic is essential as it assists the researcher to determine effectively relevant journals and articles regarding the research topic in performing in a comprehensive and comparative study for the research topic. The search terms to be implemented in the study involves "Nursing educational programs for communication in end-of-life", "nursing communication skills", "supporting patients and families in end-of-life care", "palliative care", "nursing interaction improvement in palliative care" and others. The mentioned search terms are to be customised on the basis of search to be executed in the mentioned databases regarding the study topic so that effective information is identified.
Research Question
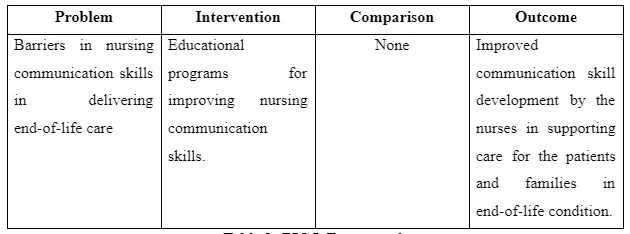
The formulation of an effective research question is essential in the study so that a proper query regarding the concerned issue in the study can be raised based on which the research is to be made to ensure enriched execution of the study. The PICO tool is to be used for formulating the research question in the study as it helps the researcher to effectively identify essential parts of the research topic to be considered in developing a proper clinical question (Patel, 2018). The PICO stands for problem, intervention, comparison and outcome. The problem is the identified clinical issue in the study for which the research is being developed (Milner and Cosme, 2017). In this study, the problem is barriers in nursing communication skills in delivering end-of-life care. The intervention is the strategies to be used for overcoming the raised problem in the study (Milner and Cosme, 2017). In this study, the intervention is educational programs for improving nursing communication skills. The comparison is referred to the contrasting of intervention to determine which of them is more potential in resolving the raised issue in the study. In this study, no comparison of interventions is to be made. The outcome is the results that are desired to be developed for resolving the raised issue in the study (Milner and Cosme, 2017). In this study, the outcome is improved communication skill development by the nurses in supporting care for the patients and families in end-of-life condition. Thus, the research question developed in the study is: Can educational programme be effective improving nurses communication skills intended to support the patient and family during end of life?
Boolean Operators
The Boolean operators are the conjunctions used in the study to link search terms or exclude keywords to develop a focused as well as productive result in the study. The operators are also used as it saves times as well as increased effort of the researcher by eliminating the irrelevant search (Majid et al. 2017). The Boolean operators to be used in the study are “AND” “OR” to improve the specificity and sensitivity of the search.
Inclusion and Exclusion criteria
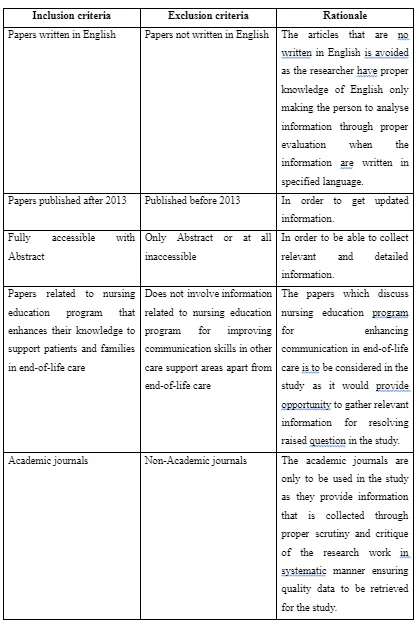
The inclusion and exclusion criteria are determined in the study to identify the characteristics to be added and the factors to be disqualified to develop a relevant and proper study. In this research, the inclusion criteria are papers written in English, published after 2013, academic journals and articles, papers related to nursing education program that enhances their knowledge to support patients and families in end-of-life care and articles that are fully-accessible. The exclusion criteria are the papers that are published before 2013, no written in English, not fully accessible, non-academic journals and articles and not involve information related to nursing education program for improving communication skills in other care support areas apart from end-of-life care. The articles that are published after 2013 is considered in the study as it is going to avoid inclusion of backdated information regarding the research topic leading to provide enhanced findings to be presented in the study that are current and relevant to the topic. The articles that are no written in English is avoided as the researcher have proper knowledge of English only making the person to analyse information through proper evaluation when the information is written in specified language. The papers which discuss nursing education program for enhancing communication in end-of-life care is to be considered in the study as it would provide opportunity to gather relevant information for resolving the raised question in the study. The academic journals are only to be used in the study as they provide information that is collected through proper scrutiny and critique of the research work in systematic manner ensuring quality data to be retrieved for the study.
Ethics
The ethics in research is important as it promotes the aim of the study that is to expand knowledge, support values needed for collective work environment and others. The ethical research also ensures the researcher has followed proper moral principles in executing the study, in turn, assuring validity and reliability of the information being presented in the study (Butts and Rich, 2019). In this study, the ethics is maintained by the researcher by providing proper relevance and credit to the authors whose information has been presented. Moreover, it is ensured that the information presented in not manipulated and influenced by personal thoughts of the researcher to ensure enriched execution of the study.
Critical Appraisal of Literature
In the end-of-life care, the nurses experience difficulties in developing communication with the dying patients and making their families consider the situation regarding end-of-life care as the feel anxious as well as unprepared in working within the settings. In the study of Leclerc et al. (2014), it is mentioned that nurses are found to communicate with the patients and family in end-of-life care without getting affected by the emotional distress of the patients and relatives. This is evident as in the study it is mentioned that 20% of the nurses are unaffected by the situation in end-of-life care and 44% do not consider sadness to be faced by the family in the condition. It has led the nurses to communicate with the patients and their family in end-of-life care with lack of empathy and compassion (Price et al. 2017). The lack of empathetic and compassionate conversation by the nurses with the patients and their families in the end-of-life condition makes the service users feel the nurses lack perception regarding their pain in turn making them feel lack of value and satisfaction in care (Yadegari et al. 2019). However, it is suggested by Leclerc et al. (2014) that inclusion of training to the nurses in end-of-life care would improve their attitudes and skills to make effective and empathetic communication. The fact regarding the importance of education or training program for the nurses to improve their communication skill in end-of-life care is supported by the study of Coyle et al. (2015). This is evident as in the study by Coyle et al. (2015) it is mentioned that a workshop is arranged for the nurses where 45 min of didactic, 90 min of small group discussion and 45 min of exemplary video of the way to interact and execute the nursing role in end-of-life care for the patients are informed. It led to improve the confidence and skills among the nurses in making effective communication as the nurses reported they understand that they are to develop effective relationship with the patients, ask open questions, acknowledge information shared by the patient and family in end-of-life condition, assess understanding of the patients and others to develop proper interaction. The study by Odachi et al. (2017) informs that understanding and acknowledging the patient’s views during end-of-life communication by the nurses makes them feel valued and respected. This is because the patients feel the nurses are effectively listening to their needs and demands which they would try to fulfil in care. In another study by O'Brien et al. (2019), it is mentioned that use of communication skill by the nurses in end-of-life of open questioning makes them gather valuable data regarding the health condition of the patient and the feedback regarding their care. This is because open questioning leads the patients to explain their hindrances and issues in details regarding care and health. Therefore, the evidence indicates that improved communication skills as achieved by the nurses in the study of Coyle et al. (2015) is effective for intending better support to the patient in end-of-life care.
In contrast, the study by Chung et al. (2016) mentioned that very low to low-quality evidence is collected in the study regarding the effectiveness of end-of-life communication training for the nurses in improving their knowledge and skill of interaction with the patients and family members. This is evident as the study mentions that out of the 20 articles selected for review regarding impact of educational intervention for nurses in improving their end-of-life communication skill only 8 articles offered supported evidence regarding improvement in communication score among the nurses in the study. Moreover, the study was unable to gather potential amount of evidence to determine whether or not effective educational intervention regarding communication by the nurses in end-of-life care affects care at the patient-level. Therefore, the study indicated that educational program may not be effective to improve communicating skills among the nurses to create better outcomes in end-of-life care for the patients and the family.
In comparison, the study by O'Brien et al. (2019) asserted that communication training to the nurses in end-of-life care is effective for them to improve their interaction skills to provide better care to the patients and family. It is evident from the study as the nurses who participated in the communication training in end-of-life care mentioned the source assisted them to understand that patience and active listening are key skills to be used in the process. This is because active listening provides the patient time and opportunity to express themselves making the nurses in end-of-life care understands the feelings and emotions along with needs and demands of the patients to be fulfilled. The similar fact is presented in the study by Mitrea et al. (2017) where the nurses on receiving communication training regarding end-of-life care mentioned they understood active listening skill is to be applied by remaining aware of personal emotions. This is to be done by remaining objective which provides opportunity to patients in sharing their personal emotions and needs avoiding the nurses to impose their thoughts. Therefore, the evidence mentions that active listening skill is potential aspects that are improved in nurses for the communication in end-of-life care of the patients and the family so that positive intended care for the patients can be provided. The study by Mitrea et al. (2017) mentioned that delivery of education regarding communication establishment by the nurses who are involved in caring in the end-of-life settings helped them understand the way interaction regarding health is to be made with the patients and family member. This is evident as the nurses in the study mentioned that they have identified more time is to be provided to patients to communicate their needs and the nurses are to remain calm and patience during the interaction for its successful establishment. This is similar to the fact presented in the study of O'Brien et al. (2019) where the nurses also claimed to have adopted the skill of patience through communication education program in the end-of-life care which led them to deliver better support to the patients. In the study by Anstey et al. (2016), mentioned that communication educational program regarding end-of-life care for the nurses mentions them to have sensitivity skills to be implemented in developing polite conversation. This is because in end-of-life condition the patients and their family are found to be in emotional distress as well as mentally unstable to accept the fact of dying. Thus, it is the duty of the nurses to have sensitivity skills in making polite conversation so that they can make the patients and their family under what is happening and develop appropriate decision regarding caring for the patients to ensure nurses are able to deliver constructive and quality care support.
The study by Markin et al. (2015) informs that education program developed in the end-of-life care settings are effective to improve communication skills of the nurses to provide better support to the patients and the family in the settings. It is evident as mean score of the nurses regarding expressing empathy, discussing treatment related to end-of-life care for patients to the families, responding to the families who do not accept the health seriousness of the patients and others are increased. Moreover, in the study, 90% of the participants mentioned they strongly agreed to the fact that the communication training in the end-of-life care settings was effective to improve care support for the patients and family. In the study Leclerc et al. (2014), the presence of effective communication establishment by the nurse in end-of-life care leads them to develop better prognosis of the diseased condition of the patients and include less aggressive medical system to be implemented for the patients nearing death.
The study by Markin et al. (2015) executed randomised controlled trial where it is informed that out of 472 trainee nurses who are randomly selected, 232 are recruited for intervention and 240 are provided usual education regarding establishment of communication in palliative care or end-of-life situation. The simulation-based intervention was seen to be effectively related with creating overall improvement in the communication skill of the nurses compared to usual care. The study also mentioned that the specific communication skills which are to be improved include discussion of spiritual issues, expressing empathy and executing care gaols in end-of-life.
In the study by Anstey et al. (2016), it is mentioned that educational programs regarding end-of-life care improve the communication skills of the nurses so that are able to make conversation which are culturally and spiritually appropriate as per the thoughts of the patients. This leads the patients to comply with the support by the nurses as they feel their spiritual thoughts are properly considered by the nurses to arrange care accordingly. Thus, it informs that the educational program does improve communication skills of the nurses in end-of-life care making them provide improved intended support to the patients and their family. In contrast, the study by Okumura-Hiroshige et al. (2018), informed end-of-life communication education to nurses indicates they to develop skills of using encouraging words. It is to make the family members and patients develop positive thoughts even their complicated health condition ensuring to create enhanced care environment. This is because in end-of-life condition patients and family members are already depressed regarding the complicated health situation and thoughts of dying. Therefore, offering hope through use of encouraging words would make them feel positive and lower their depressive which would ensure better health condition during the last days of life (Okumura-Hiroshige et al. 2018).
The study by Malik and Chapman (2017) stated that nursing education program in end-of-life condition informs the nurses to develop communication skills in using proper non-verbal communication as it acts as a powerful message. This is because use of appropriate body language along with posture and simple gestures are seen to show compassion towards dying patients. In addition, lower voice tone during conversation in end-of-life condition makes nurses show effective compassion towards the patient's condition. Thus, education program for nurses regarding communication in end-of-life condition makes the nurses improve conversation skills in letting the patients understand their pain is perceived by the nurses and they are trying to control the situation to ensure their good health. In support, the study by Pesut and Greig (2018), mentioned that nurses on availing communication education regarding end-of-life interaction expressed confidence in interacting with the patients. This indicates that education programs do create overall improvement in the nurse's skills to make better communication during end-of-life making them intended to deliver quality support to patients and their family in considering the situation and avoiding panic and fear.
Facilitators and Barriers for implementation of the findings
The implementation of education program for improving communication skills of the nurses who are intended to support the patient and their families in the end-of-life care is not going to be easy because certain barriers may be faced which would limit its implementation. As mentioned by Aldridge et al. (2016), the barrier to implement education programs for nurses regarding communication in end-of-life care includes the presence of hindered structural system in the care settings. This is because improper structure in the care settings leads the authorities unable to develop proper supervision to set effective goals and gather required resources in forming and delivering successful communication education programs for the nurses regarding end-of-life care. This issue can be resolved by changing the structure of the organisation as structural change would create alteration in way of working and management by the authorities making them develop better workflow and arrangement of resources need to establish successful nursing educational program for communication in end-of-life care.
The barrier to implement educational programs regarding communication in end-of-life care for nurses includes lack of adequate availability of experienced individuals who are educated regarding the way the programs are to be framed for its successful execution (Jennings et al. 2018). This is because presence of incapable individuals would lead to develop hindered educational program which would unable to enhance any knowledge of the nurses regarding the way to communicate with patients and their families in end-of-life care. The barrier can be resolved by identifying and recruitment of experienced health and nursing professionals from various healthcare organisations who have worked to delivery successful care and support in end-of-life condition among individuals. As criticised by Noble et al. (2018), increased funding is required for establishment of nursing education program. This is because increased amount of finite and infinite resources are needed for establishing a justified and well-structured training program. Therefore, the lack of adequate funding is acting as a barrier in establishing the findings from the study. However, it can be resolved if collaboration between two or more healthcare organisation can be developed where they are going to share the expenses for establishing communication education program for nurses in end-of-life care condition. This is because it would lower the burden of finances to be spent by single organisation in educating their nursing staffs to develop better communication skill in providing quality end-of-life care to the patients.
The barrier to be faced in establishment of the findings is the reluctance of the nurses to participate in the educational programs for improving communication skills in delivering end-of-life care. This is because the educational programs are going to require additional time and effort from the nurses to show participation and learn the new skills which the nurses may not be willing as they have long duty hours during which they are to work hard (Tirgari et al. 2016). Thus, the nurses out of work pressure and exhaustion may not be willing to invest additional time required for the successful participation in the programs. The barrier can be resolved by arranging the educational program before the working hours of the nurses on each for certain period to enhance their communication skills without increased investment of separate time for the program. The lack of proper presence of instructor-to-nurse ratio is able to create barrier towards implementation of the findings. This is because increased number of nurses to be educated or trained regarding any improvement or adoption of skill by less number of instructors leads to create work pressure on the instructors. It leads the instructors to be unable to manage the program in an effective way making them create errors and hindered or incomplete delivery of information to the learning nurses out of confusion created through work burden (Sommerbakk et al. 2016). The barrier can be resolved by recruitment of increased number of nursing instructors. This is because it would lower the workload helping the instructors to analyse and deliver information in the program in a proper way to nurses in making them adopt proper skills.
The lack of effective collaboration between the nurses and the instructors leads to create barriers in the implementation of the current findings. This is because effective collaboration makes the team of nurses and the instructors to work together in reaching a common goal through sharing of brainstormed ideas, perspectives and others. Moreover, collaboration between nurses and instructors in education programs helps to create conflict and lack of competence between one another making the nurses to proper get informed about the way their skills are to be improved in provided effective care (Brighton and Bristowe, 2016). This barrier of lack of collaboration between the instructors and nurses can be resolved by making them get properly introduced at the beginning of the program. It is to ensure they knowledge regarding one another and through initiation of discuss making them gradually develop trust to work together in the successful execution of the education program where the skills of the nurses can be effectively improved in the end.

The barriers towards the implementation of the findings that education program for the nurses help to improve their communication skill in the end-of-life care include lack of assurance and motivation to the nurses they would be able to enhance their quality. This is because lack of motivation and assurance of the nurses that their skills can be actually improved on participation in the educational program makes ignore participation as it is regarded as waste of time for them (Mandegari et al. 2018). This barrier can be resolved through formation of short-terms goals to be fulfilled in the educational program for communication skills improvement of the nurses in delivering end-of-life care. It is required so that on fulfilment of the short-term goals of learning the nurses can be self-assured that the program is effectively beneficial for them, in turn, making them show proper participation. Moreover, before the recruitment of the nurses to get involved in the program they are to be assured by the instructors through use of proper evidence regarding the way the learning process they are to get included in going to assist them to improve their communications skills in delivering end-of-life care. This is because use of evidence creates assurance, motivation and understanding among the nurses regarding the usefulness of the education program arranged for them (Nilsen et al. 2018). It, in turn, creates greater participation leading to successful implementation of education program among the nurses to enhance their skills regarding delivering care.
Continue your journey with our comprehensive guide to Nursing and Academic Practice.
Conclusion
The above discussion informs in the UK most of the patients die in the hospital and care home surroundings while being cared by the nurses. In regard to the situation, the nurses are seen to have expressed facing various issues of not being able to develop effective communication in the end-of-life condition with the patients and the family members which has made them incapable to deliver effective care during the condition. The nurses expressed due to lack of effective communication skills have led nurses become unable to provide effective emotional support to the patients and family members in end-of-life care creating prolonged bereavement and conflict attitude towards nurses by the families of the patient. Thus, the study is significant as it would shed light on whether or not education program regarding communication improves skills of the nurses to make them intend to deliver better care to patients and family members in end-of-life condition. For the purpose, the PICO tool is used to develop the research question focused on which literature search is to be made. The gathered literature informs that education programs regarding communication do create improvement on the communication skills of the nurses in end-of-life care which intends them to deliver better care to patients and support to the patient's family members. This is evident as the literature informed active listening skills, personal relationship, empathy, compassion, trust and certain non-verbal mode of communication skills is improved by the nurses in end-of-life care through education training that has intended them to deliver successful care. The literature also mentioned that better verbal communication skills were able to be established by nurses through education program regarding communication in end-of-life condition mentioning the programs has positive impact on making nurses deliver improved care through better conversation.
References
Aldridge, M.D., Hasselaar, J., Garralda, E., van der Eerden, M., Stevenson, D., McKendrick, K., Centeno, C. and Meier, D.E., 2016. Education, implementation, and policy barriers to greater integration of palliative care: a literature review. Palliative Medicine, 30(3), pp.224-239.
Anstey, S., Powell, T., Coles, B., Hale, R. and Gould, D., 2016. Education and training to enhance end-of-life care for nursing home staff: a systematic literature review. BMJ supportive & palliative care, 6(3), pp.353-361.
Banerjee, S.C., Manna, R., Coyle, N., Shen, M.J., Pehrson, C., Zaider, T., Hammonds, S., Krueger, C.A., Parker, P.A. and Bylund, C.L., 2016. Oncology nurses' communication challenges with patients and families: a qualitative study. Nurse education in practice, 16(1), pp.193-201.
Bennett, M., 2016. Nursing Care at the End of Life: 25 Years After the Passage of the Patient Self-determination Act. Journal of Hospice & Palliative Nursing, 18(6), pp.550-555.
Brooks, L.A., Manias, E. and Nicholson, P., 2017. Communication and decision-making about end-of-life care in the intensive care unit. American journal of critical care, 26(4), pp.336-341.
Brown, C.E., Back, A.L., Ford, D.W., Kross, E.K., Downey, L., Shannon, S.E., Curtis, J.R. and Engelberg, R.A., 2018. Self-assessment scores improve after simulation-based palliative care communication skill workshops. American Journal of Hospice and Palliative Medicine®, 35(1), pp.45-51.
Buccheri, R.K. and Sharifi, C., 2017. Critical Appraisal Tools and Reporting Guidelines for Evidence‐Based Practice. Worldviews on Evidence‐Based Nursing, 14(6), pp.463-472.
Chang, S.F. and Lin, P.L., 2016. Systematic Literature Review and Meta‐Analysis of the Association of Sarcopenia With Mortality. Worldviews on Evidence‐Based Nursing, 13(2), pp.153-162.
Chung, H.O., Oczkowski, S.J., Hanvey, L., Mbuagbaw, L. and You, J.J., 2016. Educational interventions to train healthcare professionals in end-of-life communication: a systematic review and meta-analysis. BMC medical education, 16(1), p.131.
Coyle, N., Manna, R., Shen, M.J., Banerjee, S.C., Penn, S., Pehrson, C., Krueger, C.A., Maloney, E.K., Zaider, T. and Bylund, C.L., 2015. Discussing death, dying, and end-of-life goals of care: a communication skills training module for oncology nurses. Clinical journal of oncology nursing, 19(6), p.697.
Curtis, J.R., Treece, P.D., Nielsen, E.L., Gold, J., Ciechanowski, P.S., Shannon, S.E., Khandelwal, N., Young, J.P. and Engelberg, R.A., 2016. Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. American journal of respiratory and critical care medicine, 193(2), pp.154-162.
Di Giulio, P., Finetti, S., Giunco, F., Basso, I., Rosa, D., Pettenati, F., Bussotti, A., Villani, D., Gentile, S., Boncinelli, L. and Monti, M., 2019. The impact of nursing homes staff education on end-of-life care in residents with advanced dementia: a quality improvement study. Journal of pain and symptom management, 57(1), pp.93-99.
Doenges, M.E., Moorhouse, M.F. and Murr, A.C., 2019. Nursing care plans: Guidelines for individualizing client care across the life span. FA Davis.
Evripidou, M., Charalambous, A., Middleton, N. and Papastavrou, E., 2019. Nurses’ knowledge and attitudes about dementia care: systematic literature review. Perspectives in psychiatric care, 55(1), pp.48-60.
Fosse, A., Zuidema, S., Boersma, F., Malterud, K., Schaufel, M.A. and Ruths, S., 2017. Nursing home physicians’ assessments of barriers and strategies for end-of-life Care in Norway and the Netherlands. Journal of the American Medical Directors Association, 18(8), pp.713-718.
Gillett, K., O'Neill, B. and Bloomfield, J.G., 2016. Factors influencing the development of end-of-life communication skills: a focus group study of nursing and medical students. Nurse education today, 36, pp.395-400.
Heravi-Karimooi, M., Rejeh, N., Garshasbi, A., Montazeri, A. and Bandari, R., 2018. Psychometric properties of the Persian version of the quality of life in early old age (CASP-19). Iranian Journal of Psychiatry and Behavioral Sciences, 12(2). Pp.67-99.
Isaacson, M.J. and Minton, M.E., 2018. End-of-Life Communication. Advances in Nursing Science, 41(1), pp.2-17.
Jafari, M., Rafiei, H., Nassehi, A., Soleimani, F., Arab, M. and Noormohammadi, M.R., 2015. Caring for dying patients: attitude of nursing students and effects of education. Indian journal of palliative care, 21(2), p.192.
Jarden, R.J., Sandham, M., Siegert, R.J. and Koziol-McLain, J., 2020. Intensive care nurses' well-being: A systematic review. Australian Critical Care, 33(1), pp.106-111.
Jennings, N., Chambaere, K., Macpherson, C.C., Deliens, L. and Cohen, J., 2018. Main themes, barriers, and solutions to palliative and end-of-life care in the English-speaking Caribbean: a scoping review. Revista Panamericana de Salud Pública, 42, p.e15.
Kinley, J., Preston, N. and Froggatt, K., 2018. Facilitation of an end-of-life care programme into practice within UK nursing care homes: a mixed-methods study. International journal of nursing studies, 82, pp.1-10.
Leclerc, B.S., Lessard, S., Bechennec, C., Le Gal, E., Benoit, S. and Bellerose, L., 2014. Attitudes toward death, dying, end-of-life palliative care, and interdisciplinary practice in long term care workers. Journal of the American Medical Directors Association, 15(3), pp.207-213.
Majid, S., Foo, S., Zhang, X., Mokhtar, I.A., Luyt, B., Chang, Y.K. and Theng, Y.L., 2017. Nurses’ information use and literature searching skills for evidence based practices. Malaysian Journal of Library & Information Science, 18(1). Pp.45-67.
Malik, M. and Chapman, W., 2017. Education and training in end-of-life care for certified nursing assistants in long-term care. The Journal of Continuing Education in Nursing, 48(2), pp.81-85.
Mandegari, Z., Bagheri, I. and Fallah Tafti, B., 2018. Palliative Care in Neonatal Intensive Care Units: Challenges and Solutions. Iranian Journal of Neonatology IJN, 9(2), pp.33-41.
Mani, Z.A., 2016. Intensive Care Unit Nurses Experirnces of Providing End of Life Care. Middle East Journal of Nursing, 101(3031), pp.1-7.
Markin, A., Cabrera-Fernandez, D.F., Bajoka, R.M., Noll, S.M., Drake, S.M., Awdish, R.L., Buick, D.S., Kokas, M.S., Chasteen, K.A. and Mendez, M.P., 2015. Impact of a simulation-based communication workshop on resident preparedness for end-of-life communication in the intensive care unit. Critical care research and practice, 2015. pp.1-23.
Masaki, H., Kawai, N., Matsumoto, K., Kuwata, M., Yoshioka, S., Nishiyama, M., Uchino, R., Nagae, H., Teshima, M., Sakai, S. and Endo, K., 2017. Consensus development of quality indicators for end‐of‐life care for elders in J apan. International journal of nursing practice, 23, p.e12562.
Milner, K.A. and Cosme, S., 2017. The PICO Game: An Innovative Strategy for Teaching Step 1 in Evidence‐Based Practice. Worldviews on Evidence‐Based Nursing, 14(6), pp.514-516.
Mitrea, N., Mosoiu, D., Ancuta, C., Malloy, P. and Rogozea, L., 2017. The impact of the End-of-Life Nursing Education Consortium International Training Program on the clinical practice of Eastern European nurses working in specialized palliative care services: a Romanian case study. Journal of Hospice & Palliative Nursing, 19(5), pp.424-434.
Montgomery, K.E., Sawin, K.J. and Hendricks-Ferguson, V., 2017. Communication during palliative care and end of life: Perceptions of experienced pediatric oncology nurses. Cancer nursing, 40(2), pp.E47-E57.
Nilsen, P., Wallerstedt, B., Behm, L. and Ahlström, G., 2018. Towards evidence-based palliative care in nursing homes in Sweden: a qualitative study informed by the organizational readiness to change theory. Implementation Science, 13(1), p.1.
Noble, C., Grealish, L., Teodorczuk, A., Shanahan, B., Hiremagular, B., Morris, J. and Yardley, S., 2018. How can end of life care excellence be normalized in hospitals? Lessons from a qualitative framework study. BMC palliative care, 17(1), p.100.
Noome, M., Dijkstra, B.M., van Leeuwen, E. and Vloet, L.C., 2016. Exploring family experiences of nursing aspects of end-of-life care in the ICU: A qualitative study. Intensive and Critical Care Nursing, 33, pp.56-64.
O'Brien, M.R., Kinloch, K., Groves, K.E. and Jack, B.A., 2019. Meeting patients’ spiritual needs during end‐of‐life care: A qualitative study of nurses’ and healthcare professionals’ perceptions of spiritual care training. Journal of clinical nursing, 28(1-2), pp.182-189.
Odachi, R., Tamaki, T., Ito, M., Okita, T., Kitamura, Y. and Sobue, T., 2017. Nurses' experiences of end-of-life care in long-term care hospitals in Japan: Balancing improving the quality of life and sustaining the lives of patients dying at hospitals. Asian nursing research, 11(3), pp.207-215.
Okumura-Hiroshige, A., Fukahori, H., Yoshioka, S., Kuwata, M., Nishiyama, M. and Takamichi, K., 2018. Effect Of An End Of Life Nursing Education Program On The Attitudes Of Clinical Nurses Caring For Older Adults In Japan. Innovation in Aging, 2(suppl_1), pp.523-523.
Omar Daw Hussin, E., Wong, L.P., Chong, M.C. and Subramanian, P., 2018. Nurses’ perceptions of barriers and facilitators and their associations with the quality of end‐of‐life care. Journal of clinical nursing, 27(3-4), pp.e688-e702.
Patel, D.I., 2018. Nursing Research, CER, PICO and PCORI. Journal of community & public health nursing, 4(1). Pp.90121.
Pesut, B. and Greig, M., 2018. Resources for educating, training, and mentoring nurses and unregulated nursing care providers in palliative care: a review and expert consultation. Journal of palliative medicine, 21(S1), pp.12-50.
Price, D.M., Strodtman, L., Montagnini, M., Smith, H.M., Miller, J., Zybert, J., Oldfield, J., Policht, T. and Ghosh, B., 2017. Palliative and end-of-life care education needs of nurses across inpatient care settings. The Journal of Continuing Education in Nursing, 48(7), pp.329-336.
Richards, D.A., Hanssen, T.A. and Borglin, G., 2018. The second triennial systematic literature review of European nursing research: Impact on patient outcomes and implications for evidence‐based practice. Worldviews on Evidence‐Based Nursing, 15(5), pp.333-343.
Sommerbakk, R., Haugen, D.F., Tjora, A., Kaasa, S. and Hjermstad, M.J., 2016. Barriers to and facilitators for implementing quality improvements in palliative care–results from a qualitative interview study in Norway. BMC palliative care, 15(1), p.61.
Tamaki, T., Inumaru, A., Yokoi, Y., Fujii, M., Tomita, M., Inoue, Y., Kido, M., Ohno, Y. and Tsujikawa, M., 2019. The effectiveness of end-of-life care simulation in undergraduate nursing education: A randomized controlled trial. Nurse education today, 76, pp.1-7.
Threapleton, D.E., Chung, R.Y., Wong, S.Y., Wong, E.L., Kiang, N., Chau, P.Y., Woo, J., Chung, V.C. and Yeoh, E.K., 2017. Care toward the end of life in older populations and its implementation facilitators and barriers: a scoping review. Journal of the American Medical Directors Association, 18(12), pp.1000-1009.
Tirgari, B., Forouzi, M.A., Razban, F. and Alimirzaei, R., 2016. Difficulties felt by intensive care unit nurses in providing end-of-life care in Southeast Iran. Journal of Hospice & Palliative Nursing, 18(5), pp.443-449.
Travers, A. and Taylor, V., 2016. What are the barriers to initiating end-of-life conversations with patients in the last year of life?. International journal of palliative nursing, 22(9), pp.454-462.
Yadegari, M., Rankin, J. and Johnson, J.M., 2019. Nurses’ communication with dying children and their families in pediatric oncology: A literature review. Journal of Nursing Education and Practice, 9(2). Pp.56-90.
What Makes Us Unique
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



