Prevalence of Prostate Cancer in the U.S.
Introduction
Since 1984, prostate cancer has been the most common non-cutaneous cancer in men in the United States and today represents a quarter of all these cancers. The estimated lifetime risk for this disease is 16.72%, with a risk of death of 2.57%. Prostate cancer is rarely diagnosed in men under the age of 50, who account for only 2% of all cases. The average age at diagnosis is 68 years and 63% of cases are diagnosed after 65 years of age.. (Kavousi & Andrew Novick, 2014)
ANATHOMY & PHISIOLOGY
The base of the prostate is at the bladder neck and the apex at the urogenital diaphragm. The Denonvilliers’ fascia, a thin, filmy layer of connective tissue, separates the prostate and seminal vesicles from the rectum posteriorly. Skeletal muscle fibers from the urogenital diaphragm extend into the prostate at the apex and up to the midprostate anteriorly. The peripheral zone comprises all the prostatic glandular tissue at the apex as well as all of the tissue located posteriorly near the capsule. In this zone, carcinoma, chronic prostatitis, and postinflammatory atrophy are relatively more common than in the other zones. The central zone is a cone-shaped area of the adult gland, with the apex of the cone at the confluence of the ejaculatory ducts and the prostatic urethra at the verumontanum. The transition zone consists of two equal portions of glandular tissue lateral to the urethra in the midgland. This portion of the prostate is involved in the development of age-related benign prostatic hyperplasia (BPH) and, less commonly, adenocarcinoma. The anterior fibromuscular stroma (AFMS) forms the convexity of the anterior external surface. The apical half of this area is rich in striated muscle, which blends into the gland and the muscle of the pelvic diaphragm. Toward the base, smooth muscle cells become predominant, blending into the fibers of the bladder neck. The distal portion of the AFMS is important in voluntary sphincter functions, whereas the proximal portion plays a central role in involuntary sphincter functions. The histologic architecture of the prostate is that of a branched duct gland. Two cell layers, a luminal secretory columnar cell layer and an underlying basal cell layer, line each gland or duct. The lumens of otherwise normal prostatic glands and ducts frequently contain multilaminated eosinophilic concretions, termed corpora amylacea, that become more common in older men. Calculi are larger than those corpora with a predilection for the ducts that traverse the length of the surgical capsule, separating the transition and peripheral zones. The prostatic capsule is composed of fibrous tissue surrounding the gland. Although the term “capsule” is embedded in the current literature and common parlance, there is no consensus about the presence of a true capsule. This capsule is best appreciated posteriorly and posterolaterally as a layer more fibrous than muscular, between the prostatic stroma and extraprostatic fat. (Hammerich & Wheeler, 2018)


FUNCTIONS
Prostate function unknown - secretory
Testosterone required for normal function
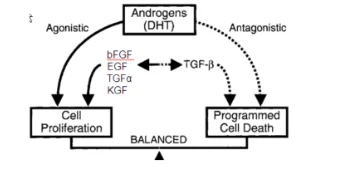
Permissive role for growth; androgen withdrawal = prostate involution
Majority of serum testosterone from testis – unbound T bioavailable form
DHT formed within prostate epithelial cells – 40x more active vs. T
DHT diffuses to stroma (most of the androgen receptors; paracrine effect) Stromal nuclei produce growth factors
Growth factors drive epithelial cells
Stimulatory bFGF, KGF (FGF-7) and EGF* and IGF (80%) TGFα (20%)
ETIOLLOGY
Take a deeper dive into Nursing Role in Fall Prevention with our additional resources.
Although the specific cause of the initiation and progression of prostate cancer is not yet known, there is considerable evidence that genetics and environment play a role in the origin and evolution of the disease. Firm epidemiological evidence suggests that prostate cancer has a genetic and familial component. The results of a meta-analysis showed that the relative risk increases according to the number of affected family members, their degree of relationship and the age at which they were affected (Zeegers y cols., 2003). Infections are estimated to cause nearly 20% of all cancers in the world (American Cancer Society, 2008). Chronic inflammation leading to cellular hyperproliferation to replace damaged tissue contributes to the development of cancers associated with inflammation of the colon, esophagus, bladder, and liver The accumulation of epidemiological, histological, and genetic evidence suggests that a similar process may underlie the development of prostate cancer. Some evidence suggests that prostate cancer could have an infectious etiology. Two meta-analyzes examining 34 case-control studies reported that there is a statistically significant association of prostate cancer with a history of sexually transmitted infection. Inflammatory infiltrates and the histological lesion called prolinerative inflammatory atrophy (AIP) are common in clinical samples of the prostate. AIP is a spectrum of lesions characterized by epithelial atrophy, a low apoptosis index and a high proliferation index, usually associated with inflammatory infiltrates. (Kavousi & Andrew Novick, 2014)
Other influencies:
Sexual activity
It is hypothesized that sexual activity exposes the prostate to infectious germs, which may increase the risk for prostate cancer, similar to what happens in women with the causal relationship between HPV and cervical cancer.
CLINIC PRESENTATION
In general, patients are asymptomatic or show symptoms of urinary voiding and/or storage related to PC. These involve decreased urinary stream, pushing, frequency, urgency and vesical tenesmus. Advanced PC symptoms include bone pain, renal failure, hematuria, pathological bone fractures, physical exhaustion and weight loss. The most significant tools for PC diagnosis are PSA levels (>4 ng/ml) and a suspicious digital rectal examination (DRE) (e.g., increased consistency or nodules). However, other factors can also increase PSA levels in the absence of PC: ejaculation, trauma (e.g., rectal, transurethral catheter placement), inflammation and infection (acute prostatitis), as well as prostatic hyperplasia. There can be significant inter-individual variation; thus, at least two measurements taken at least 3 weeks apart are required. (Castillejos-Molina & Gabilondo-Navarro, 2015)
DIAGNOSIS
PSA:
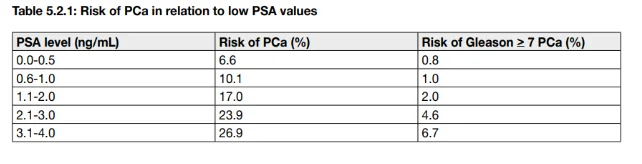
The use of PSA as a serum marker has revolutionised PCa diagnosis. PSA is organ- but not cancerspecific, therefore, it may be elevated in benign prostatic hypertrophy (BPH), prostatitis and other nonmalignant conditions. As an independent variable, PSA is a better predictor of cancer than DRE or transrectal ultrasound. Serum PSA levels increase with tumour stage, although they are limited for accurate prediction of final pathological stage. PSA is produced by benign and malignant tissue, thus, there is no direct relationship between serum PSA and clinicopathological tumour stage.
PROSTATE BIOPSY:
The need for prostate biopsy is based on PSA level and/or suspicious DRE. Age, potential comorbidity, and therapeutic consequences should also be considered and discussed beforehand . Risk stratification is a potential tool for reducing unnecessary biopsies. Limited PSA elevation alone, should not prompt immediate biopsy. PSA level should be verified after a few weeks using the same assay under standardised conditions (i.e., no ejaculation, manipulations, and urinary tract infections) in the same laboratory . Empiric use of antibiotics in an asymptomatic patient in order to lower the PSA should not be undertaken. (NICE, 2019) Ultrasound-guided biopsy is now the standard of care. A transrectal approach is used for most prostate biopsies, although some urologists prefer a perineal approach. Cancer detection rates are comparable with both approaches
IMAGENOLOGICAL DIAGNOSIS
ECOGRAPHY
Prostate volume can be calculated using different formulas. Volume calculation requires measuring up to three dimensions of the prostate. In the axial plane, the transverse and anteroposterior dimensions are measured at the point of maximum transverse diameter. The longitudinal dimension is measured in the sagittal plane, just outside the midline, because the bladder neck can mask the cephalic extension of the gland. The average mature prostate weighs between 20 and 25 g, and remains relatively constant until around age 50, when the gland increases in size in many men. When a more precise determination of the volume of the gland is required, for example during brachytherapy, planimetry can be used. With the patient in the lithotomy position, the probe is mounted in a stepped device and serial cross-sectional images are obtained at preset intervals (eg, 3-5 mm) through the entire length of the gland. The surface area of each serial image is determined and the sum of these measurements is then multiplied by the total length of the gland to obtain the volume of the gland.
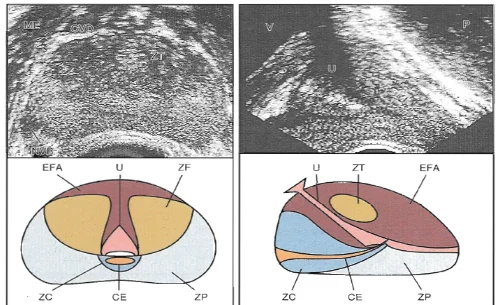
Once the gland volume has been obtained, derivatives such as PSA density (PSAD = serum PSA / gland volume) can be calculated. A high density of whole-gland PSA has been shown to have a sensitivity and specificity of 75 and 44%, respectively, in predicting a positive diagnosis of cancer on repeat biopsy (Djavan y cols., 2010). Unfortunately, there is high interoperator and intraoperative variability in PSA density determinations, and similar predictive information can now be obtained using the ratio of free PSA: total PSA in serum. In general, transition zone benign prostatic hyperplasia nodules are hypoechoic, although they may contain isoechoic or even hyperechoic foci. A hypoechoic lesion is malignant in 17% to 57% of cases (Frauscher et al., 2012), highlighting the need for biopsy, although it is recognized that they are not pathognomonic for cancer, as was once considered. Any focal abnormality of the contour of the outer edge of the gland and any asymmetry of the echotexture of the peripheral zone of one lobe with respect to that of the other are recorded. Focal loss of typically bright white periprostatic fat suggests extracapsular spread of prostate cancer, although it is not well visualized if present as a microfocus.
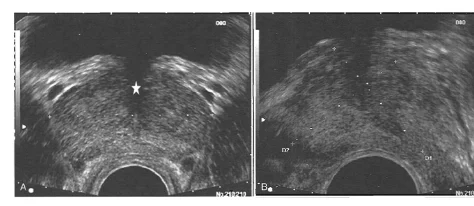
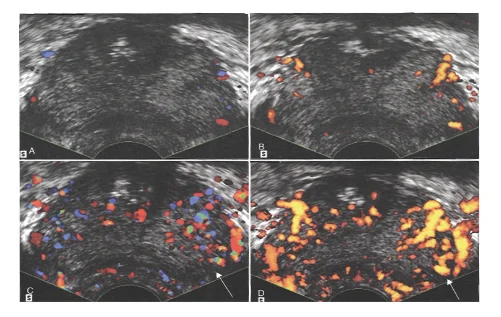
DOPPLER ECOGRAPHY
Color Doppler imaging is based on the change in frequency of the reflected sound waves relative to the insonation frequency and, therefore, represents the blood flow velocity in a direction-dependent manner . Color assignment is based on the direction of blood flow associated with the orientation of the transducer receiving the signal; Flow approaching the transducer is shown in shades of red, and flow away from the transducer in shades of blue; the color is not specific to arterial or venous flow. Patients with detectable Doppler flow within their dominant tumor at the time of transrectal ultrasound-guided biopsy have a 10-fold increased risk of PSA recurrence after radical retropubic prostatectomy. Likewise, increased flow was associated with a higher Gleason score, higher incidence of seminal vesicle invasion, and a lower biochemical disease-free survival rate compared to subjects without increased flow on preoperative transrectal ultrasound (50% versus 96% without biochemical disease at 31 months) (Ismail et al., 2017). Other researchers have also shown the association of power Doppler flow signals as an indicator of microvascular density, with a higher Gleason score, and have suggested a correlation with prognosis. (Kavousi & Andrew Novick, 2014)
CAT & MRI
Computed tomography (CT) and magnetic resonance imaging (MRI) to assess the local extent of disease and the possibility of lymph node involvement are not routinely recommended, due to low sensitivity Cross-sectional imaging studies can be reserved for high-risk patients, such as those with a clinical stage greater than or equal to T3 disease or a probability greater than 20% by nomogram of lymph node metastasis. Due to the rarity of lymph node involvement in contemporary populations studied, there appears to be an overuse of imaging studies Combined MRI and MR spectroscopy have been evaluated for prostate cancer staging, although there is no evidence that these methods overcome the current limitations of microscopic disease visualization Specialized techniques, such as high-resolution MRI used in tandem with intravenous administration of lymphotropic superparamagnetic nanoparticles, may allow the detection of small, otherwise undetectable lymph node metastases in patients with prostate cancer (Harisinghani et al., 2003). However, these techniques require additional clinical evaluation before their widespread use (Kavousi & Andrew Novick, 2014) T2-weighted imaging (WI) remains the most useful method for local staging on MRI. At 1.5T (Tesla), MRI has low sensitivity for detecting extraprostatic extension of carcinoma (22-82%) or SVI (0-71%), but higher specificity (61-100% and 62-100%, respectively) [161-176]. Global MRI accuracy for distinguishing T1/T2 stages from T3 stage is 50-85%. These disappointing results are because MRI cannot detect microscopic extra-prostatic extension. Its sensitivity increases with the radius of extension within periprostatic fat. In one study, the EEC detection rate increased from 14 to 100% when the radius of extension increased from < 1 mm to > 3 mm. In another study, MRI sensitivity, specificity and accuracy for detecting pT3 stage were, 40, 95 and 76%, respectively, for focal (i.e. microscopic) extra-prostatic extension, and 62, 95 and 88% for extensive extra-prostatic extension. An endorectal coil improves staging accuracy at 1.5T, and accuracy of 77-83% has been shown for combined endorectal and external coils vs. 59-68% for external coil alone. Dynamic contrast-enhanced imaging combined with T2-WI may also improve local staging . The high field strength allows highresolution T2-WI. and results at 3T seem better than at 1.5T, even if the experience of the reader remains of paramount importance, MRI accuracy at 3T varies between 67% and 93% depending on the experience of the reader. Even if MRI is not perfect for local staging, it may improve prediction of the pathological stage when combined with clinical data . Given its low sensitivity for focal (microscopic) extra-prostatic extension, mpMRI is not recommended for local staging in low-risk patients. However, mpMRI can still be useful for treatment planning in selected low-risk patients. (European asociation of urology, 2015)
BONE SCINTIGRAPHY
Bone scan is the most sensitive modality for the detection of skeletal metastases (Terris et al., 1991). Skeletal radiographs are less sensitive for identifying distant spread and are often used only to confirm a positive bone scan in men at low risk for bone metastases. Because metastases are rare at the time of diagnosis in asymptomatic men in the era of PSA, the systematic practice of bone scan in this population can give false positive results, with the consequent anxiety and unnecessary costs (Chybowski y cols., 2011). Consequently, recent guidelines recommend requesting a bone scan in patients with a PSA greater than 20 ng / mL, a Gleason score of 8 to 10, clinical stage T3 or T4, or clinical symptoms (National Comprehensive Cancer Network,2009).

Metastatic nature of the lesions needs to be checked by other imaging modalities. The NPV for bone scanning is 87-100%. Its diagnostic yield is significantly influenced by the PSA level, the clinical stage and the tumour Gleason score and these three factors were the only independent predictors of BS positivity in a study of 853 patients . BS positivity rate is extremely low (< 1%) in low-risk patients , In contrast, it is 6.6-38.5% in patients with PSA level of 20-50 ng/ mL, 19-90.7% in patients with stage > T3 and 16.9-29.6% in patients with Gleason > 8 tumours . The proportion of positive BS in patients with PSA level of 10-20 ng/mL (1-33.3%) or Gleason 7 (2.8-22%) is quite variable from one study to another. In two studies, a major Gleason pattern of 4 was found to be a significant predictor of positive BS (European asociation of urology, 2015)

TREATMENT
The surgical treatment of PCa consists of radical prostatectomy (RP). This involves removal of the entire prostate gland between the urethra and bladder, and resection of both seminal vesicles, along with sufficient surrounding tissue to obtain a negative margin. Often, this procedure is accompanied by bilateral pelvic lymph node dissection. The goal of RP by any approach must be eradication of disease, while preserving continence and whenever possible potency. There is no age threshold for RP and a patient should not be denied this procedure on the grounds of age alone . However, patients with a life expectancy of > 10 years are more likely to benefit from the procedure. Increasing comorbidity greatly increases the risk of dying from non-PCarelated causes. An estimation of life expectancy is paramount in counselling a patient about surgery . Currently, RP is the only treatment for localised PCa to show a benefit for OS and cancer-specific survival (CSS), compared with conservative management, as shown in one prospective randomised trial. During 23.2 years of follow-up, the SPCG-4 trial showed that RP was associated with a reduction of all-cause mortality. The relative risk (RR) of death at 18 years was 0.71 (95% CI, 0.59-0.86). The number needed to treat (NNT) to prevent one death at 18 years of follow-up was 8; the NNT decreased to 4 for men younger than 65 years of age. Radical prostatectomy was also associated with a reduction in PCa-specific mortality at 18 years (RR = 0.56; 95% CI, 0.41-0.77). The benefit of surgery with respect to death from PCa was largest in men younger than 65 years (RR, 0.45) and in those with intermediate-risk PCa (RR, 0.38). However, RP was associated with a reduced risk of metastases among older men (European asociation of urology, 2015)
REFERENCES
Castillejos-Molina, R. A. & Gabilondo-Navarro, . F. B., 2015. Prostate cancer.
European asociation of urology, 2015. Guidelines on Prostate cancer.
Hammerich, K. & Wheeler, T., 2018. Anatomy of the prostate gland and surgical pathology of prostate cancer. s.l.:s.n.
Kavousi, L. & Andrew Novick, 2014. Campbell-Walsh Urology. 11 ed. s.l.:s.n.
NICE, 2019. Assessing suspected prostate cancer. NICE GUIDELINES.
NICE, 2019. Prostate cancer: diagnosis and management. NICE GUIDELINES.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



