Implementing PCC in Mental Healthcare
CHAPTER 1
1.0 Introduction
The essentials of nursing care practice in undergraduate nursing care are to enhance the student’s ability to provide quality care to individuals regardless of their challenging or complex behaviour. One issue that emerged during the course period is the inability of nurses, supervisors and support staff involved in care practice to adopt person-centred care (PCC) approaches within the healthcare setting. Yet, Barksdale et al (2014) emphasizes the importance of adopting PCC approaches when dealing with issues affecting the individuals they care for.
A closer evaluation of the organization’s routine staff training program reveals the lack of PCC as one of the items the staffs are trained on. Therefore, the proposed quality improvement (QI) project focuses on improving the practice of person-centred approaches by training the staff on how to develop organizational systems and leadership that is centred towards delivering a PCC approach to mental healthcare.
Person-centred care has been described in a variety of pieces of literature as an important element of care for nursing care patients (Brownie & Nancarrow 2013, Burns & Grove 2009). Also termed as patient-centred care (PCC), the concept of person-centred care traces its roots in North America during the 1980s where it emerged as an approach for improving the lives of individuals with intellectual disabilities (Claes et al, 2010). Since then, according to Davis et al (2005), PCC has gained a worldwide popularity as a method for improving and changing the way people with intellectual disabilities are provided with opportunities and choices to practice self-determination while under care. Duffy & Sanderson (2004) observed that the use of person-centred care contributed to an improvement of the quality of services delivered to intellectual disabilities and contributed to positive healthcare outcomes. Besides, researchers (e.g. Epstein & Street 2011) have recommended person-centred care by insisting that care should be delivered in a manner that considers the receiver’s unique characteristics.
The initiative of the proposed QI project will take place in a long-term care hospital located in an urban setting in London. The target organization is an aid-funded facility equipped with facilities for people with intellectual disabilities and delivers home-based care programs to a few individuals with intellectual disabilities. The facility has direct support professionals, nurses and certified intellectual disability professionals who work to provide a wide range of care services such as care coordination, disease management, health promotion, health maintenance and community services.
An observed lack of regular staff training on PCC in the target organization implied that the staff were not up to date with effective PCC approaches nor did they have the knowledge on the importance of PCC within the mental healthcare setting. Consequently, the service users did not have an opportunity for self-determination in decisions regarding their well-being. For example, the researcher observed that most clinical appointments were planned by clinical officers without the involvement of the targeted service user. Furthermore, there was a reported increase in behavioural outbursts by the organization’s incident management committee. While some efforts had been made by the Local Authority Disability Department to provide training on basic on principles of PCC, the training was only offered to upper and middle management. In fact, in the organization where this QI project is intended to take place, 150 direct support staffs (i.e. nurses and professional intellectual disability care nurses) with the responsibility of coordination and provision of immediate care were not involved in the training. Besides, there were no plans to assist these care providers acquire these skills of practice.
The Francis report (Halligan, 2013) revealed serious gaps in the provision of quality care to people with intellectual disability. This report identified a serious gap between the quality of care the patients received and the quality of care they were supposed to receive. Furthermore, the report expounded on the important roles of direct support staff in delivering quality care aimed at achieving positive health outcomes, which directly depends on the trainings they receive from their respective organizations. Ideally, service users with intellectual disability deserve the opportunity to self-determination and to take part in their own care planning (Frampton et al, 2008). However, according to Epstien & Street (2011), it is impossible to achieve this objective without training the direct support staff on the process of self-determination, which is a significant element of PCC.
An effective way of delivering education is through knowledge translation. Knowledge translation can assist in ensuring that the targeted organization and the community at large understand and adopt effective PCC approaches. Grove & McIntosh (2005) observed that PCC has been linked with social inclusion and the ability of patients to participate in healthcare decision making. Therefore, the proposed QI project is an educational initiative that will ensure that healthcare workers have effective training on the principles of PCC in the delivery of healthcare services to people with intellectual disabilities.

1.1 Structure of the Project Proposal
After the introduction, the next chapter will give a background of the project – setting the context and providing background information on PCC. Thus, chapter two will review existing literature and contextualize PCC. Chapter 3 will describe the proposed improvement plan. Here, there will be a description of the improvement in detail while giving evidence-based justification. Furthermore, the improvement section will explain the contexts and terms of the proposed improvement - ending up explaining how the improvement will be implemented and the specific theories to be considered when implementing the improvement. Chapter four will describe the research methods that will be used in implementing the project. Here, the proposal will describe the data collection methods, the participants to be included in the project, their settings and why they are to be included. The next chapter, chapter five, will describe the ethical considerations to be made during the project implementation. It will consist of description of at least four ethical principles relating to the PIP. Chapter six and seven will describe the research dissemination methods and project timeline respectively.
Chapter 2
2.0 Background
Dig deeper into Problems with Adult Nursing Practice with our selection of articles.
From time immemorial, caring for people with intellectual disability has been an emotional affair, and most workers providing care to such patients have been over-protective of the individuals they care for (Hafskjold et al, 2015). According to Hobbs (2009), the workers perform for the patients most tasks associated with daily living, and this has been the best approach to care. While providing the type of care that most workers think is the best for the patients, they might ignore the patient’s response to this care (Holburn et al, 2004). Patients with intellectual disabilities are entitled to be viewed as ‘normal’ , and in fact, this led to the development of the term “normalization,” whereby workers are asked to understand the patients beyond their disabilities and treat them as normal human beings with the same entitlement to opportunities, dignity and respect as anyone else (Parish, 2005). Consequently, a change has been noticed in the recent past, where agencies providing care to people with disabilities have adopted person-centred planning as a requirement for practice (Taylor & Taylor, 2013). However, according to Taylor & Taylor (2013) these changes have only been implemented to meet the agencies’ requirements and not for the sake of nurturing self-determination for people with intellectual disability. The researcher is aware that in 2015 some staff members in the targeted organization received some exposure to person-centred thinking but did not get practical skills on how to develop staff training in a manner that enhanced implementation and understanding of best PCC approaches. Yet, Holburn & Vietze (2002) insists that direct support staff must understand the processes involved in enhancing self-determination in order to deliver quality care to their patients. Yet, according to White & Dudley-Brown (2012), there is a strong correlation between patient safety and the quality of care delivered by healthcare practitioners.
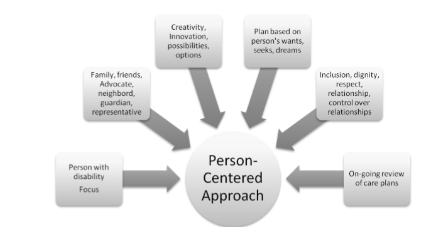
In the UK, it is estimated that at least 1.5 million people live with learning disabilities, including 905,000 adults of age 18 years and above (Foundation for People with Learning Disability, 2019). While there are no clear estimates of the actual costs of caring for people with learning disabilities in the UK, research by Ervin & Merrick (2014) show that people with learning disabilities tend to seek care at advanced stages of their conditions, thus resulting to high cost of care. In 2001, a white paper published by England’s department of Health emphasized that people with learning disabilities require adequate support to enable them to engage in self-determined actions (England Department of Health, 2001). As highlighted in figure 1 below, the PCC model of care encourages and allows people to get involved in their care and take control of their lives within the care setting (Maeng et al 2012). The National Health Service (NHS, 2019) stipulates that PCC should revolve around maintaining the patient’s respect and dignity, adequate information sharing with patients and their families, inter-professional healthcare collaboration to improve quality of care, and inclusion of patients and their families in the decision-making process. Research evidence in existing literature propose the idea that the implementation of PCC based on solid and stepwise training of practitioners can improve the health outcomes of people with intellectual disability. According to Michigan Department of Community Health (2010) and Viau-Guay et al (2013), adopting person-centred approaches in long-term care for people with intellectual disabilities can create a significant improvement in the patient’s healthcare outcomes.
Similarly, Claes et al (2010) realised that skill and knowledge development among healthcare workers on person-centred approaches is important to general practice. The main aim of the present QI project is to develop the skills and knowledge of healthcare workers on person-centred approaches to care so that they can easily empower patients and involve them in their own care planning. By using person-centred strategies, the workers will be able to increase the patients’ satisfaction levels within the care setting. With this regard, Barksdale et al (2014) stipulated that healthcare workers should not view such changes as additional tasks but rather as a learned behaviour that should be infused into the organizational culture. Therefore, a proper integration of the culture of PCC into the organization will require the staffs to change their mindset on how they approach the healthcare delivery and to maintain the interest of the patient at the forefront of care practice.
Continue your exploration of Problems Associated with Adult Nursing Practice with our related content.
2.1 Person-Centred Planning
Developing an effective person –centred plan begins with the adoption of person–centred thinking. At least 1.5 million people in the UK have been diagnosed with intellectual disability. They should be accorded equal rights and provided with equal rights to accessing quality care with their non-disabled counterparts. Thus, the proposed project will develop a person-centred plan to involve people with intellectual disabilities in meaningful activities and to accord them the dignity they deserve. Developing an educational curriculum (see appendix 2) that supports person-centred planning will enable the program recipients (i.e. staff) to acknowledge and recognise the patient’s cultural beliefs, choices, as well as to match the staff’s specific skills with the patients’ needs (Epstein & Street 2011). When patients’ opinions and preferences are valued, they find an opportunity to be involved in objective activities that enhances their healthcare outcomes (Claes et al, 2010). Furthermore, according to Barksdale et al (2014), allowing patients to be part of the decision making concerning their health care enables them to express what is important to them rather than just accepting what the staffs think is important to them. Moreover, person-centred planning provides an opportunity for the staffs to make a difference in the patients’ lives by enhancing and incorporating their perceptions in the care process. For instance, during my placement, I saw that nursing intervention, medication administration and follow-up appointments may become problematic because the patients’ or client’s inputs are not sought. Hence, the implementation of person-centred planning allows patients feel respected, valued and feel like they have a greater effect on their well-being while reducing incidences associated with acting out behaviour (Hafskjold et al, 2015). But, as asserted by Barksdale et al (2014), training staffs on the principles and practices of person-centred planning may only be effective if it includes a redefinition of culture, identification and solving problems related to learning culture, and reshaping of patient-worker communication.
2.2 Organizational communication and culture
According to Hobbs (2009), communication is a significant area that may be a barrier to effective delivery of patient care within most disability care settings. In simple terms, communication involves information sharing between a sender and receiver (Epstein & Street 2011). Communication could be done verbally, through signs, expressions and drawings, and an effective communication between carers and patients can improve their healthcare outcome (Claes et al, 2010). However, patients with learning disabilities have other comorbidities that make effective communication difficult and therefore most of them have many unmet needs (Hafskjold et al, 2015). Consequently, according to Hobbs (2009), it is important for staffs to understand and interpret alternative means of communication such as communication charts, sign language and gestures so that patients with learning disabilities can receive effective care. Barksdale et al (2014) postulate that person centred care is a continuous activity, which means that the healthcare providers must have enough training to understand the importance and proper application of person-centred practices. Hafskjold et al (2015) observe that staffs communicate with patients by issuing commands and imperatives, yet such means of communication are not in line with the principles of person-centred communication principles. Instead, a person-centred communication occurs when both parties (i.e. patient or worker) supply information to the other regarding what they want, understand, feel, desires or perceives (Epstein & Street 2011). Without taking time to understand the patient’s wishes, preferences and choices, effective communication does not exist. With this regard, Barksdale et al (2014) noted that a repeated disregard to the patient’s preferences and wishes leads to patient frustration and consequently an explosive expressions and behaviours by the patient, which may also cause injuries. Hobbs (2009) argued that poor communication between patient and workers has negative impacts and occurs as a ‘missed opportunity,’ which is attributable to exerting excessive power over patients. Therefore, workers should be accountable for any disruptive or problematic incidence that could have been avoided by listening to the clients. To prevent patients’ explosive behaviour, the management should provide workers with the necessary training and tools for understanding their roles within the care setting. Therefore, an evidenced-based training intervention on person-centred practices will supply staffs with the skills for encouraging and supporting patients with intellectual disability, thereby enhancing their self-determination and improving their healthcare outcomes. However, Hobbs (2009) observed that developing a practice improvement for enhancing PCC may encounter numerous challenges that must be dealt with. The authors postulated that healthcare organizations should maintain the application, development and implementation of PCC to create a proper culture of care.
The implementation of PCC in healthcare organizations is significantly influenced by organizational culture, the workers’ learning culture, as well as the environment within which the care is delivered (Hafskjold et al, 2015). Hence, to successfully implement the proposed QI project, the researcher will rely on ‘change theories’ and ‘PCC coaches’ who may positively influence the organization’s culture and support its learning culture respectively. Ideally, an effective provision of PCC requires healthcare workers to understand the meaning of ‘person-centred,’ which basically means providing care according to an individual’s beliefs, culture, preferences, choices and desires (Claes et al, 2010). An effective practice of PCC requires that patients must be the centre of attention by allowing them to make an input in the decisions related to their healthcare. Thus, according to Hobbs (2009), staffs must acquire cultural competency through training so that they can understand how PCC influences effective care. According to the Department of Disability Services and Developmental disabilities Administration, long-term care providers must include end of life planning as part of the individual support plans (ISP) for patients with intellectual disability (Epstein & Street 2011). However, according to observations by Barksdale et al (2014), many workers involved in developing the ISP find it uncomfortable to initiate such conversations with their patients. With proper training on PCC principles, healthcare workers involved in ISPs can find it easier to implement end of life planning and any other routine responsibilities that they find challenging to engage in. The importance of PCC in all aspect of care cannot be overemphasized. According to Hobbs (2009), PCC enables the delivery of effective support to patients and their families even during challenging moments, and therefore staffs should have proper training on PCC delivery especially when the patients and their families are experiencing such challenging events.
2.3 Organization Learning Culture
Individuals have different learning cultures, and this can influence the implementation of the proposed QI project. An emphasis will therefore be put on learning styles while training staff so that the learning culture does not affect the implementation of PCC principles in the targeted organization (Claes et al, 2010). Hafskjold et al (2015) describe organizational learning culture as each person’s perception and reaction to learning and is associated with the way members of the organization may respond to innovations, mistakes, and tensions, as well as how they conceptualize the achievement of the desired learning outcomes. In an ideal organizational learning culture, all staffs would be ready and excited to work and initiate the innovations (Epstein & Street 2011). On this note, studies by Senge (2006) and McCormack (2007) present the importance of a positive learning culture in enhancing the staff’s readiness and willingness to implement and maintain the practice of person-centred principles. Planning is an important healthcare practice. Hobbs (2009) asserted that person centred planning is likely to yield positive outcomes due to the collaborative nature of the process. Hafskjold et al (2015) also indicate that person centred planning creates an opportunity to for staffs to share and transfer knowledge because it requires them to be more alert in identifying patient preferences. Several studies (e.g. Robertson et al 2004, Holburn et al 2004, and Hlburn 2002) have confirmed the association between person centred planning and improved outcomes compared to the implementation of PCC without an accompanying person-centred plan. Furthermore, Hobbs (2009) postulates other importance of person-centred planning such as patient satisfaction and mutual respect among the staffs. The plans laid down during the person-centred planning are usually implemented in person centred care. Resmond et al (2012) and McCormack et al (2011), while studying the topic of person-centred care, suggested that the implementation of person-centred care in most health organizations is conducted based on two models, namely the logic model and the Kurt Lewin’s change model, the former being used in evaluating the PCC’s effectiveness. Ideally, this is a confirmation that an effective implementation of the person-centred plan depends on the Staff’s preparedness and the leadership’s ability to communicate, facilitate and provide leadership for change within the organization.
The parson-centred care model focuses on the patient as the recipient of delivered care. Ideally, if it is effectively implemented, the patient can experience a multidimensional positive effect because it targets at providing a meaning to different care activities that contribute to an increase in the patient’s sense of worth (Epstein & Street 2011). Besides, according to Hobbs (2009), staffs are likely to feel a sense of accomplishment when they notice the change that they bring in the patient’s life through PCC. Consequently, both the patient and the staff benefit in the sense of patient satisfaction and job satisfaction respectively. Also, according to Hafskjold et al (2015), PCC enhance the interdisciplinary collaboration among staffs as they must coordinate to deliver patients’ needs. The collaboration and its continuity are achieved by minimising patient movement within the hospital, empowering staff to engage in activities that improve patient outcome and providing autonomy to the patient (Claes et al, 2010). Consequently, staffs become more ready to implement PCC. Thus, the proposed PCC training project will specifically be about guiding the participants on how to deliver the process of PCC. There are four items considered to be elements of PCC namely; individualised approaches to care, valuing and value, individual perspectives, social and positive environments (Patton, 2005). The proposed QI training project will focus on these items to ensure that the participants are equipped with the knowledge of how to exercise these items.
2.4 PCC and Nursing
The NMC (2015) considers PCC as one of the important professional standards and competencies for all practicing nurses. Ideally, nurses are expected to adhere to patients’ preferences, and this should include any relative or family member directly responsible for the patient; to promote the delivery of quality care. The NMC recommendation implies that all nursing curriculums must give priority to person-centred care so that new nurses are prepared with the skills that enable them to appreciate, practice and coordinate PCC (Epstein & Street 2011). Barksdale et al (2014) insisted that nurses have an important role to play in delivering PCC. The author argued that that regardless of the patient’s disabled status; they deserve to be integrated into the care planning process. This is because patients tend to appreciate it when included in making important decisions regarding their healthcare, and when the decisions are significant to the well-being (Claes et al, 2010). Therefore, nurses have the responsibility of empowering patients to participate in creating their own care plans using appropriate communication tools. In this sense, the nurses assume the role of advocates who should have the necessary skills to identify and interpret behavioural responses as a way of communicating with patients with limited speech or effective communication abilities (Hafskjold et al, 2015). Fundamentally, the practice of PPC assumes that healthcare delivery process is standardized and offers an equal opportunity for all patients to receive quality care (Epstein & Street 2011). When Small and Small (2012) tested the PCC model of care at Cleveland Clinic, they realised that an effective implementation of PCC requires that nurses must properly be trained to change their mind and embrace a new way of caring, which is characterised by constant patient-nurse/caregiver interactions. The Institute of Medicine (IOM, 2001), under the topic: Cross the Quality Chasm, pinpointed PCC as one of the key quality improvement aspects within the healthcare system. Since then, a variety of scholars have evaluated the nature of PCC and how it can be effectively integrated into the healthcare system. For instance, Hobbs (2009) observed a poor conceptualization of PCC among his study participants and concluded that such a poor conceptualization hindered practitioners from effectively implementing PCC approaches. Furthermore, according to Hobb’s (2009) evaluation, nurses play an important role in patient interaction, and that when PCC is properly implemented, it can lead to an increase in patient satisfaction and improved quality of care. Part of the proposed project’s aim is to enhance the nurses’ conceptualization of PCC.
But, Hobbs (2009) argues that implementing an effective PCC approach within any care setting requires a gradual change in the organizational culture, as opposed to a one-off change. This explains why there are still significant inconsistencies among organizations regarding the most effective manner of contextualizing PCC. Nonetheless, Barksdale et al (2014) acknowledge some factors influencing the implementation of PCC approaches as the physical environment, staffs’ learning environment, and organizational culture. When these factors are well considered, the organization’s staffs are more likely to consider PCC as a standard of practice rather than an additional task for nurses and other employees (Claes et al, 2010). This implies that if the staffs are guided on how to implement PCC approaches, it would be easier to standardize the approaches into the normal healthcare systems.
2.5 PCC for the intellectually disabled
For a while now, most healthcare institutions have applied PCC approaches in caring for people with intellectual disabilities, as a way of normalizing the care they receive (Epstein & Street 2011). Furthermore, according to Hobbs (2009), PCC is vital in caring for people with learning disabilities because such patients require the nurses’ direct support to have their needs addressed. Thus, caring for people with learning disabilities cannot be possible without adopting PCC approaches. Whereas there is not clear definition of the role of nurses in providing PCC for people with learning disabilities, Barksdale et al (2014) argue that staffs should give an opportunity for the patients to have a say in the decisions regarding their healthcare. Thus, they have the responsibility of encouraging and supporting their patients to achieve self-determination and make decisions regarding their care. Moreover, according to Robertson et al (2005), some patients with intellectual disabilities refuse care when they are not offered with choices to make. Hence practitioners have applied PCC approaches in long-term care to improve patient outcome and experience. However, Hobbs (2009) argues that PCC approaches are only useful in long term care when the staffs are comfortable with adopting PCC, if the staffs are well trained on PCC approaches and when there is an effective implementation plan. A study by Viau-Guay et al (2013) used open-ended questionnaires on 392 participants to evaluate the relevance of a PCC implementation plan. The study found that the application of PCC approaches was useful to nursing care workers. However, the workers had little knowledge on how to maintain the application of PCC approaches in practice. The study therefore highlighted the importance of training and knowledge transfer to influence change of practice. The background of the study has identified various aspects of person-entered practice that can be applied within the organization. We have justified the need for an evidence-based educational intervention that will guide the participants on how to plan and apply PCC within the care setting. Generally, the reviewed literature has revealed that some persons with learning disabilities may not be receiving the care they deserve as a result of staff members not being trained on PCC approaches. This implies that practitioners who handle patients with intellectual disabilities should receive continuous training on person-centred planning, so that the principles and approaches of PCC are sustainably applied within the care setting. According to Hafskjold et al (2015), the extent to which an organization develops a learning culture defines how well the organization implements and sustains the use of PCC approaches in care. On the same note, Hafskjold et al (2015) argued that the development of proper leadership and culture will can create an enabling environment for staff members to be motivated in supporting the people they care for, thus enhance PCC. The gap that the proposed QI project will address will enable the targeted organization to effectively provide person-centred care.
In the above sections, the author has discussed the approach to the proposed QI educational initiative for PCC, Moreover, there is description of the multidisciplinary team, the theoretical background, ethical consideration, implementation process and the evaluation mechanism of the proposed project. But first, the following is a statement of the underlying problem.
2.6 Statement of the problem
This QI project intends to address the problem of non-inclusion of person-centred approaches in staff training curriculum within the target organization. Apart from being equipped to provide a person-centred approach of care, current research (i.e. Maeng et al 2012, Barksdale et al, 2014) emphasize that direct support staff should involve patients and other clients in decisions regarding their care. Moreover, Maslow et al (2013) argue that staff training is a vital component of employee development towards the practice of PCC approaches. As observed by the researcher in this QI project, the target organization currently has no staff training program that equips the direct support staff on the principles of PCC. According to Claes et al (2010), person-centred planning provides an opportunity for patients to express their thoughts and ideas to be included in care strategies. Hence, training the staff who work closely with patients on how to recognize patient preferences will enable them to understand how to incorporate those preferences in the patient care plans (Barksdale et al, 2014). Barksdale et al (2014) observed that some individuals with learning disabilities can hardly express themselves as a result of their disabilities. However, when direct support staff are properly trained on how to communicate and understand the behaviours of such patients based on person-centred approaches, the patients can be allowed self-determination and easily be incorporated in decision-making (Barksdale et al, 2014).
2.7 Purpose statement
The main aim of the proposed project is to improve quality of service delivery to people with intellectual disability by developing an educational initiative on Person-centred care. The project will use an evidence-based educational program to fill the gap between the lack of PCC practice and the existing evidence-base on the importance of PCC in improving quality of care for people with intellectual disability (Viau-Gay et al 2013).
2.8 Project objectives
To promote self-determination in patients with intellectual disabilities
To ensure maximum benefit for people with intellectual disability form PCC
2.9 Project Justification
Upon completion, the proposed QI project will improve the health outcomes of people with intellectual disabilities through evidence-based educational training. The training program will equip attendees with practical skills in promoting the principles of PCC and self-determination of patients under their care. Claes et al (2010) argued that developing a training plan for training mental healthcare staffs on PCC approaches is an effective way of translating knowledge into practice, thereby promoting a widespread adoption of PCC practices within the nursing care setting. Moreover, the proposed project will help in developing an information base for direct support workers on how they can support patients with complex mental health issues who could also be struggling with issues of situational transitions (McCormack & McCance, 2006). The proposed project intends to integrate a program for implementing the person-centred care practice into the training program and this will strengthen the policies that enhance the normalization of patients with intellectual disabilities (Barksdale et al, 2014). A significant objective of PCC is to promote effective care that is within the patients’ preferences and values. Therefore, the proposed project resonates with the suggestions by Claes et al (2010) on the need for the implementation of new evidence-based practices to improve the quality of care delivered to patients. According to Smith-Stoner (2011), taking a collaborative approach in the delivery of healthcare will provide an opportunity to eliminate disability stigmatization and instead present care to the person regardless of their disability.
2.10 The project Team
Pelzang (2010) defines a team as a group of people coordinating and working together to achieve the same objective. Therefore, a team may not be as effective as desired if they are just randomly selected (Kelly, 2014). But rather, an effective team is developed with a careful selection of individuals joining that team. Therefore, in the proposed project, the researcher will select each team member based on their qualifications, skills, knowledge and ability identify the need for change; and participate in the change initiative in the most professional and effective way. As the project leader the researcher will exercise their leadership skills by developing methods of team engagement through a variety of strategies, activities and skills. First, as recommended by Porter et al (2003), the researcher will use back up behaviours, which entails anticipating for the team’s needs and balancing their workload so that they are relieved of the pressure accompanying the change process. Secondly, the researcher develops an adaptability skill, which is defined by Cannon et al (1995) as the ability to adjust initial plans, resources and behaviours based on new and emerging information from team members. Furthermore, the researcher will be attentive to identify any need for improvement by keenly monitoring the team’s internal and external environment.
2.11 Team meetings
There will be a weekly team meeting every Friday from 2pm to 4pm, whose main agenda will be to discuss the project’s progress any emerging issues and the necessary inputs for enhancing the project implementation process. Stanhope et al (2015) argued that leadership plays an important role during the implementation of person-centred care in healthcare settings. Similarly, Stanhope et al (2015) asserted that the use of PCC protocol for staff training can effectively benefit from transformational leadership because PCC is an on-going process that needs to be maintained with good leadership to ensure that the team is continuously empowered. Therefore, as a leadership aspect, the researcher will observe the importance of holding effective team meetings. As postulated by O’Deal et al (2006), team meetings should be goal-driven and should produce a positively oriented synergy between the team members. The meetings will be face to face, held on specific location at specific time. Chairing the meetings, the researcher will contact all team members in prior, to gather any information that would be useful in developing the meeting agenda. This assumes that the success of every meeting will be dependent on how good the project leader is prepared and conducts the meeting. Kelly (2013) conducted a research on healthcare team meetings and found that the success of such meeting also depends on how the chairperson keeps control of the meeting right from the meeting conception to the time the minutes are approved. Thus, to maintain control of the meeting, the researcher will adopt a comprehensive meeting preparation, efficiently use the meeting environment, and effectively manage team members’ participation (Hafskjold et al, 2015). Therefore, to achieve effective meeting outcomes the researcher will send each team member the meeting agenda beforehand.
2.12 The project Rationale
However much educational knowledge and ability healthcare providers may have, patients have the right to be involved in any decision made regarding their care and should be the point of reference for any care plane designed for them (McCance et al 2011). In 2001, the UK’s Department of health published a white paper acknowledging that people with learning disabilities may not be handed with the respect and dignity they deserve as evidenced by their behaviours, which are attributable to their state of disability (Robertson et al 2005). Therefore, the white paper suggested that all staffs in the learning disability care setting should undergo a person-centred care training aimed at improving care quality by enhancing their ability to implement PCC approaches and principles. Therefore, as part of the response to this recommendation, the researcher will convene an effective team capable of developing a comprehensive education curriculum aimed at training the staffs on the approaches to PCC in caring for people with learning disability. To affirm this rationale, Pelzang (2010) asserted that developing an effective curriculum for training healthcare staff on person-centred planning ensures that the staffs adopt a standardized and consistent practice of PCC. Pelzang (2010) proposed a variety of leadership abilities and styles that nursing graduates must have in order to implement an effective service improvement initiative within healthcare organizations. Furthermore, graduate nurses are not only trained on nursing care but also on the identification and satisfaction of patient needs. Therefore, the researcher argues that nursing practice. In the proposed project, the researcher takes an approach that leaders must identify effective ways of managing resources well enough to balance the equilibrium between quality and productivity. Furthermore, the researcher believes that a successful implementation of the project will require an accurate evaluation of costs to ensure that the project runs on a sound financial and economic planning.
Chapter 3
3.0 The improvement
The proposed quality improvement project is aimed at changing the way people with intellectual disability are cared for in the nominated organization. The change agent will assemble and lead a team of stakeholders, a representative of the patients and other members of the organization. The change agent will then engage in an extensive review of literature to identify evidence-based research on PCC. Meanwhile, the team will consist of the project team leader, a representative of registered nurses, a certified intellectual disability professional, and a person-centered care coach; and will meet once a week for six weeks to discuss issues pertaining to the project and develop a consensus on various issues related to the applicability and implementation of the project. The team will also receive a synthesis and analysis of literature for evaluation. Particularly, the main purpose of the analysis will be to guide the team as they develop the education initiative by focusing on various concepts and principles of PCC.
3.1 Project Assumptions
Ideally, assumptions are statements that could be wrong or right because there is no evidence to support them (Grove et al 2013). Before the project implementation, the change agent will make the following assumptions regarding its outcomes:
Intellectual disability patients want to feel respected and valued by participating in their own care
Nurses and other healthcare staff always want to engage in best practices when caring for their patients
Training protocols are effective ways of helping learning disability nurses and other staff to learn new practice skills
An effective implementation of PCC can increase patient satisfaction and improve the lives of persons with intellectual disability
These assumptions will be useful in evidence-based projects because they help in effective understanding of the issue at hand, thereby helping to move the project forward (Grove et al, 2013). Furthermore, these assumptions will help in determining the most effective project design.
3.2 Scope of the project
The proposed educational program will be extended to nurses handling patients with intellectual disability, support staff and any other staff member interacting with intellectual disability patients in their line of care duty.
3.3 Expected outcomes
Upon completion, the project is expected to improve the health outcomes of people with intellectual disability through an evidence-based staff training program. Participants of the training program will end up with the knowledge and self-determination to facilitate patients’ participation in their own care. According to Maslow et al (2013), training programs are effective approaches for passing the knowledge of PCC principles to nursing staff and facilitating the translation of than knowledge into practice. Therefore, the training program will:
Promote a widespread use of PCC approaches and principles in the daily delivery of care to persons with intellectual disability.
Be a source of knowledge to health workers on how to manage patients with complex health issues.
Integrate PCP implementation program into the training curriculum to develop a policy of and normalize the practice of PCC when caring for patients with intellectual disability.
These outcomes are in support of an earlier report by Institute of Medicine (2001) emphasized the implementation of new evidence-based practices to improve the safety and quality of care delivered to patients.
3.4 Project implementation process
The author will assume project leadership role to oversee all activities and processes involved in the project. Besides, the author will apply organizational leadership techniques and interpersonal relationships to develop the organizational culture for purposes of enhancing the proposed innovation. Next the author will begin the project by assembling the team consisting of qualified intellectual disability professionals, nurses and other stakeholders such as the target organization’s management team. The author, as the project manager, will then assign a timeline to the project, within which various project milestones should be achieved as well as the project evaluation should be done. The project manager will also engage in an analysis and synthesis of the evidence-based research on PCC, before conducting a comprehensive review of literature evidence on person-centred planning, the delivery of educational curriculum on PCC, as well as the most appropriate training protocol for the project. Also, part of the planning will be an updating of the currently existing PCC policy in the target organization, and an evaluation of the proposed training protocol and curriculum. The project manager will then evaluate the content of the pre-test and post-test items before developing the PCC implementation plan based on Lewin’s change theory.
3.5 The training
The training, curriculum delivery and implementation of person-centered thinking will be led by a person-centered coach. Other roles of the coach will be to help leaders and staff members understand the use of various PCC approaches, the application of those approaches in various clinical situations and the impact of those approaches on patient well-being. Moreover, the coach will be expected to identify whether the current organizational practices can accommodate the application of PCC approaches and suggest any suitable practice amendments (e.g. change in policy and procedures). The coach will also participate in advocating for positive behavioral change among the staff. Meanwhile, the training curriculum will be delivered once a week – for six weeks during the staff normal staff meeting sessions. During each session, the coach will offer the structured curriculum and allow time for participants to discuss among themselves and ask questions. At the end of the six weeks, each participant will be required to fill a post-test questionnaire for evaluating the project’s impact on their PCC knowledge.
3.6 Project evaluation
The main aim of the QI project is to promote PCC for people with intellectual disability thereby improving the health outcomes of patients receiving health services within the organization. An elaborate project evaluation will be developed and implemented to ascertain the overall success of the training program because data can be used to evaluate the project’s progress or compare the project’s success with outside metrices (Kelly, 2014). The proposed project will rely on the logic model. According to Howard (2011), the logic model entails a framework that measures the relationship between activities, resources and the outcomes. The use of this model will allow the change agent to identify and communicate the nature of the intervention and its results while emphasizing the relationship between the two. Based on the logic model, pre-test a post-test evaluation will be conducted to measure the extent to which the training program has improved the staff’s knowledge on PCC. As illustrated in appendix 3, the pre-test and post-test evaluation questionnaire will seek to identify the participants knowledge of PCC approaches before and after the training by gauging the extent to which they understand key terms in PCC, the impact of PCC on the provision of healthcare, the impact of caregiver’s conduct on patient’s well-being, the role of social inclusion in PCC and the role of informed decision-making on the patient’s well-being. The pre-test questionnaire will be taken at the beginning of the training while the post-test questionnaire will be administered twice: at the 3rd week and at the 6th week. The latter will be useful in identifying any need for revising the curriculum.
3.7 Using theory to support change
The change agent will use the Lewin’s change model to explore how training the staff will contribute to a change of PCC practice within the organization. In a study by Deci & Ryan (2012), the researchers explored the self-determination theory and noted how autonomy can be used to enhance patients’ ability to confidently adopt new behaviours such as stopping cigarette smoking. A similar approach will be taken in the proposed project, where PCP will be used to improve patients’ self-determination, teaching patients how to be independent and participate in their own care. By letting the staffs learn about the proposed change early enough, the change agent will create an opportunity for a smoother change implementation process. With this regard, according to White & Dudley-Brown (2012), change is mostly resisted because the people involved in the change process do not feel involved in the decisions leading up to the change process. The following section illustrates how the Lewin’s change model will be used to support the change process and minimize change resistance:
3.7.1 Unfreezing
In the unfreezing stage of the implantation process will be characterised by an engagement of all stakeholders that represent the target organization. Force field analysis will be used in identifying some of the factors that might interfere with the implementation process, especially those that are related to nurses’ workload, complexity of required care and the organization’s culture. Furthermore, the change agent speculates that if policies are revised to support leaders in their duty of promoting PCC, then it is highly likely that the staffs will fully embrace the change.
3.7.2 The Move
This stage will majorly involve maintaining equilibrium between the change restraining issues and the available resources. Therefore, some of the factors that will encourage the ‘move’ stage include redistribution of workload to provide time for the education participants, financial recognition, and redistribution of coaches’ workload to allow them participate in the project.
3.7.3 Refreezing
After the change implementation, the target audience shall have understood the importance of PCC and communicated the same information to patients and other stakeholders. The organization will be advised to acknowledge good results by rewarding staffs that have done well in adhering to the principles of PCC. According to White & Dudley-Brown (2014), this implies the need for an effective measurement and control system that enables the leadership to conduct an on-going monitoring. The proposed QI project is aimed at improving the practice of PCC in learning disability health care setting, thereby contributing to the improvement of quality services to those under the target organization’s support. In this context, Kelly (2014) observes that a variety of data can be used to measure and monitor the intervention’s effectiveness. Upon initiating the improvement, there will be a need for constant progress evaluation, to ensure that the change is sustained. Therefore, the logic model, proposed by Hodges & Videto (2011) will be used in identifying the curriculum’s effectiveness. Hodges & Videto (2011) observe that the logic model (appendix 4) enables the change agent to effectively communicate the various activities involved in the intervention, as well as the main goal of the intervention. In support of the logic model, Parchman & Howard (2011) described it as the relationship between activities, resources and the outcomes within the confines of a specific objective or goal. Therefore, the model will particularly be used in hypothesizing the curriculum outcomes.
Chapter
4.0 Methodology
4.1 Introduction
Research methods are the tools and instruments used to achieve the study results (Bowers, et al., 2007). Highlighted in this chapter are the design, approach, data collection and sampling techniques that will be used in achieving the objectives of the proposed QI project. Therefore, the chapter will contain an account of the research tools and methods that will be used to deliver and evaluate the proposed education program. Furthermore, this section will highlight the rationale behind every method as well as how they fit for use in the proposed project.
4.2 Research Approach
Research approaches define the comprehensive methods and assumptions used in collecting, analyzing and synthesizing data to come up with conclusive results (Al-Benna, et al., 2010). The choice of research approach is determined by the research topic under investigation and can be divided into data collection and data analysis approaches (Giuliano & Polanowicz, 2008). According to Spiers, et al. (2012), the data collection approaches can be categorized into qualitative and quantitative approaches while data analysis approaches can either be deductive or inductive. Quantitative approaches are often used to objectively measure the relationship between variables using mathematical, statistical or numerical data analysis techniques (Packer-Muti, 2009). They focus on collecting and analyzing numerical data to explain or measure the relationship between variables. On the other hand, qualitative approaches focus on gathering subjective data through narratives and stories to identify the respondents’ perceptions, opinions or attitudes towards a phenomenon (Ramakantan, 2007). In the proposed project, the researcher will rely on quantitative research approaches to achieve the project objectives. Particularly, quantitative approaches are considered appropriate for the project because they will facilitate the evaluation of the participant’s knowledge of PCC approaches. The main aim of the proposed project is to improve the knowledge and practice of PCC within the organization through an education intervention. Therefore, the project will rely on quantitative approaches (i.e. Measures of central tendencies such as mean, mode and median) to evaluate the participant’s knowledge of PCC approaches before and after the education intervention. By using quantitative approaches, the project will be able to gather the participants’ scope of knowledge of PCC. This will not only facilitate curriculum development but also help in identifying specific areas of policy revision within the organization to favor PCC. More importantly, quantitative approaches will facilitate the development of a practice philosophy that is anchored on experiences and practice processes reinforced by literature and evidence-based knowledge.
4.3 Data collection and analysis
Having selected quantitative approaches for use in the proposed project, many data collection tools can be used to collect data e.g. interviews and questionnaires (Panagiotakos, 2008). However, to evaluate the participant’s knowledge of PCC before, during and after the education intervention, the project will rely on pre-test and post-test questionnaires. As opposed to interviews where both the interviewer and interviewee must be available thus time consuming, questionnaires take less time to execute because the respondent can answer the question at their convenience (Al-Benna, et al., 2010). Furthermore, analyzing the questionnaire would take less time and resources than interview responses because in the latter case, the researcher will need to transcribe the data before analyzing (Bowers, et al., 2007). The questionnaires will be used as the pre and post-audit tools for gauging the participants’ knowledge of PCC. Each participant’s score of the questionnaires will be gathered and analyzed to determine their scores using simple measures of central tendencies (i.e. mean). Participants will be required to partake the same questionnaires before, during (at week 3) and after the education intervention (at week 6). The average scores will then be compared to determine the change in knowledge.
4.4 Sample selection
As earlier identified, the proposed QI project aims to improve the practice of PCC by educating the nursing staff of the selected organization on principles and practice of PCC when caring for learning disability patients. To achieve this objective, a sample of staff will be selected to attend the training program. Particularly, the sample selection will focus on staffs responsible for handling patients with learning disability in their daily routine of practice. Therefore, the project will adopt a purposive sampling approach, which is a form of non-probability sampling that entails identifying study participants based on the researcher’s judgment of their suitability to participate in the study (Giuliano & Polanowicz, 2008). Because the purpose of the project is well-known, purposive sampling is considered most appropriate as it will allow the change agent to choose the most appropriate staff to participate in the education program. We expect at least 10 learning disability staffs to enroll for the education program.
Chapter 5
5.0 Ethical issues
This chapter will highlight the various ethical considerations that will be made during project development and implementation. According to the Nursing and Midwifery Council (NMC, 2015), there are specific ethical considerations in nursing research that must be made to safeguard the interest and safety of all the participants involved. Furthermore, the ethical practice has become a central subject in nursing research that is used to determine the validity and reliability of the studies/projects (Buchanan & Zimmer, 2012). Moreover, ethical considerations would be required to make the fundamental basis for decision-making. Specifically, ethical issues include informed consent, privacy, and protection from harm. In the proposed PIP, the potential relationship between the researcher and the participants give rise to various ethical issues that must be considered. For instance, throughout the project, the ethical principles of non-maleficence, beneficence, truthfulness sand confidentiality must be considered. While the principle of beneficence inspires the researcher to represent the participant’s interest all the time (Lo & Parham, 2009), the principle of non-maleficence requires the researcher to do good in all aspects of the project (Morris & Dracup, 2007). Within this context of non-maleficence, the researcher causing either physical or psychological harm to the participants. Furthermore, the project will adopt an effective data storage and dissemination strategy to promote non-maleficence. Meanwhile, there are general ethical considerations that will be made to adhere to the above-mentioned ethical principles. For instance, the researcher will seek informed consent from all the participants before enrolling them to partake the questionnaire. This is to ensure that their participation is fully voluntary as recommended by (Jones, 2012). Furthermore, b seeking informed consent, the researcher will have an opportunity to explain the questionnaire content and why it is important to take part in the pre-test and post-test questionnaires. More importantly, all the participants will be protected from any form of sexual harassment, physical abuse, stress or embarrassment by maintaining a high level of integrity, mutual respect and cooperation during the training program. This part of the adherence to non-maleficence and beneficence ethical principles.

Chapter 6
6.0 Data analysis and presentation of results
The main aim of the proposed quality improvement is to develop and deliver an education intervention aimed at enhancing the practice of PCC in hospital care setting. The aims will be achieved alongside various goals including enhancing an equal accessibility of care within the organization, enhance the patients’ self-determination within the care setting and ensuring that patients gain the maximum benefit from PCC. In the end, we expect the project to yield specific outcomes including a completely revised training policy, well developed training sessions, a pre-test and post-test framework and an effective implementation and evaluation plan. As part of the results, this section will predominantly present the data analysis and results presentation methods. Furthermore, this section will discuss the potential strengths and weaknesses of the project, the implementation and evaluation plans of the project and the project’s contribution to professional development. Moreover, this section will highlight the applicability of the quality improvement intervention, how the project’s results will impact on healthcare practice, research and policy; as well as the impact of the project on the society.
6.1 Literature review
With regards to literature review, the researcher will conduct a comprehensive literature review with the aim of developing a well-analysed and synthesised evidence-base for the implementation of PCC in mental healthcare setting. To achieve this, the change agent will apply the Walden literature review matrix. Beforehand, the change agent will share the matrix with three content experts for a preliminary evaluation before presenting it to the project team members to receive their opinion with regards to its acceptance and applicability in the project. The literature review process will also include an evaluation of the quality of evidence. Therefore, the literature and quality of evidence will be evaluated and graded based on the John Hopkins Nursing Evidence-Based Practice Rating Scale. Meanwhile, the content experts will review the literature matrix to ascertain that they will yield rich and relevant evidence to guide the project implementation. The expert’s comments will then be shared with the project team to as part of the input in the development of the curriculum plan. Meanwhile, the literature review results will be presented in textual content. The literature text will be organized in thematic form by grouping related data under specific codes, then grouped under specific themes. Through thematic presentation, it would be easier for content experts to evaluate the literature and identify any relevant or irrelevant content. The second expected result is a revised training policy. Here, the change agent will present the current training policy to the project team members and pinpoint the existing gaps. This will involve the identification of several issues including the fact that the current policy, based on the change agent’s evaluation, does not include all staff members. Rather, the policy only addresses direct support professionals, going by the practice that such policies must address all members of the organization taking part in the planning and implementation of care processes. Therefore, while revising the training policy, the change agent will emphasize that all the nurses and other staffs involved in the care process should be included in the policy because they will all be trained on an annual basis after the initial training during hiring. Meanwhile, the DDA training policy for direct support professionals (DDS, 2013) will be used with person-centred thinking introduced in all its four stages except the second stage that focuses on individualized specialized training.
The third expected outcome, the curriculum session protocols will be based on a planned and systematic implementation strategy. First, the protocol will be the guiding framework during the training implementation. Ideally, the protocol will entail a stepwise tool developed for maintain high standards of PCC care. The standards will be conceptualized as the use of evidence and maintenance of consistency during the entire training process. Therefore, by using a protocol in delivering the curriculum, the change agent will ensure that there is consistency within the entire project through delivery of same training level across the organization. As part of the implementation process, the protocol framework for the curriculum delivery will define the protocol’s purpose, the curriculum’s seven-module content, and each module’s tittle the module’s mode of presentation, evaluation process and training time frame. Furthermore, the protocol will give a complete description of the procedures and guidelines to follow when to ensure that the curriculum is consistently delivered across the organization. Meanwhile, the change agent will also ensure that the protocol is evaluated so that its applicability and relevance to the organization’s policy is determined beforehand. The fourth outcome will be the educational curriculum. The proposed educational curriculum will be developed after a comprehensive review of literature on PCC practice and the positive impact of implementing PCC in similar care settings. Meanwhile, the researcher will obtain an IRB approval from the University before collecting any data involved in the project. The curriculum content will be subjected to an expert evaluation aimed at validating its ability to pass quality skills and knowledge. The experts will be selected based on their skills and experiences in the delivery of disability care services, nursing leadership and expertise in PCC implementation and management. The effectiveness educational curriculum will be evaluated through an aggregate score of the participants’; knowledge test questionnaires. For example, the project will be considered successful if all the participants register an above 50% improvement in the post-intervention knowledge test compared to pre-intervention knowledge test. The results will be presented in tabular format. Perhaps the most important outcome of the QI project is the implementation and evaluation of project plan. After presenting the implementation plan to the project team and making the aware of the long-term and short-term outcomes they are supposed to pay attention to during the project evaluation, the team will be expected to identify specific issues such as organizational culture that may have a negative impact on the project implementation process. As recommended by Kelly (2014) one way that the change agent can address such an issue is involving the team early enough. Meanwhile, to evaluate the project implementation process, the team will be expected to identify items such as organizational culture and learning styles as some of the factors that could affect the project implementation. In fact, White & Dudley-Brown (2012) demonstrate how the Lewin’s change model can help in identifying the factors that can enhance of affect the project implementation program, including organizational culture, staffs learning abilities and workload. That said, both the implementation and evaluation will be instrumental in measuring the outcome of the change process. With this regard, the long-term and short-term outcomes will be evaluated by the departments to identify its impact on each department.
6.2 Summative Evaluation
The change agent will also use a summative evaluation process through qualitative means, which according to White & Dudley-Brown (2012) entails the measurement of project outcome and the project team’s achievements. Ideally, this evaluation process will be meant to identify areas of improvement as well as opportunities for growth. At the end of the final project team meeting, the change agent will introduce a summative evaluation questionnaire consisting of question items meant to evaluate the stakeholder’s participation and involvement in the curriculum plan development and revision of the training policy; the change agent’s leadership of the entire project; and the content, products and processes of the quality improvement project. The team members will then me requested to return the questionnaires through mail. There are specific themes that the change agent will look up to in the returned questionnaires. First, there will be a keen focus on the team’s deliberations over the change agent’s leadership as a student. Secondly, the change agent will be keen to identify whet the team thinks about the curriculum, and their opinion on what will be considered a success of the curriculum plan. Ultimately, this thematic data will support the intended outcome of the project.
6.3 Dissemination
In evidence-based practice, dissemination of research and practice improvement projects is considered an important part of the research process because it is only through dissemination of the results that the project/study findings will be received and implemented by the target audience (Brownson et al, 2018). Getting the work published in a journal might be time-consuming and a bot challenging considering that most learning disability journals receive many contents for publication and might not have enough room to publish the results of the proposed project. Thus, the change agent will supplement the poster presentations with other formal presentation that are more accessible and will create more opportunity for consumption of the project’s content. Nonetheless, any available opportunity to present the project’s result will be explored as an excellent way to get feedback (Al-Benna et al 2010). This will include presenting the results to my lectures and fellow students for feedback before any formal publication of the results. Upon completion, the QI project will be disseminated through a scientific poster. According to Rabin & Brownson (2017), a design poster is a communication tool that visually relays information to the target audience through visually appealing cues such as pictures and diagrams. Therefore, the poster, as part of the dissemination plan, will include the project tittle, project objectives, and a summary of the research methods, finings and conclusion. There are several reasons why posters will be considered the best dissemination media for the proposed quality improvement project. For instance, posters can be presented in different events and used in several times (Rabin & Brownson 2017). Furthermore, according to Rabin & Brownson (2017), posters can be distributed to the target audience to pass the message without the author’s presence. This will be especially advantageous to the target organization because they can be printed and pinned on walls within the organization to pass the information to a larger audience.
Other dissemination options that will be explored include presentation at learning disability professionals’ conference, professional roundtable talks and other forms of oral presentation. When preparing for the oral presentation, the change agent will be keen to get the details of how long the presentations will take and whether the audience expect visual aids such as slideshows or videos during the talk. Nonetheless, the change agent will endeavor to conduct a thorough practice beforehand to ensure that the key conclusion points are addressed within the allowed time. In case an opportunity for oral presentation presents itself, the change agent will avoid the temptation of spending too much time on the background and literature review section and instead acknowledge that the audience might only be interested in key elements of the project such as the project’s objectives, methodological approach, key outcomes and applicability to practice.
References
- education for advanced nursing practice. Washington DC: Author.
- American Nurses Association, (2014). Education opportunity: Patient/family centered care.
- Barksdale, D. J., Newhouse, R., & Miller, J. A. (2014). The patient-centered outcomes Research
- Bostrom, R. P., Anson, R., & Clawson, V. K. (1993). Group facilitation and support systems. In:
- Jessup L. M. Valacich J. S. (Eds), Group support systems: New perspectives (pp. 146–
- aged-care facilities: A systematic review. Clinical Interventions in Aging, 8, 1.
- Burns, N., Grove, S.K. (2009). Strategies for promoting evidence-based nursing practice. In N.
- Burns, S.K. Groves (Eds.), The practice of nursing research (pp. 616-622). St. Louis,
- Brownson, R. C., Colditz, G. A., & Proctor, E. K. (Eds.). (2018). Dissemination and implementation research in health: translating science to practice. Oxford University Press.
- Cannon-Bowers, J. A., Tannenbaum, S. I, Salas E., & Volpe, C. E. (Eds.). (2001). Defining
- Claes, C., Van Hove, G., Vandevelde, S., van Loon, J., & Schalock, R. L. (2010). Personcentered
- Davis, C. B., Cornman, C. B., Lane, M. J., & Patton, M. (2005). Person-centered planning
- Driskell, J. E., & Salas, E. (1992). Collective behavior and team performance. Human Factors: The Journal of the Human Factors and Ergonomics Society, 34(3), 277-288.
- Dukes, E., & Sweeney, J. (2009). Recognizing the value of involving service users with intellectual disability in healthcare planning: A bottom-up approach is the best way to inform policy development and deliver person-centered provision, argue Eileen Dukes and John Sweeney. Learning Disability Practice, 12(10), 33-37.
- Epstein, R. M., & Street, R. L. (2011). The values and value of patient-centered care. The Annals of Family Medicine, 9(2), 100-103.
- Flynn, A.V., & Sinclair, M. (2005). Exploring the relationship between nursing protocols and nursing practice in an Irish intensive care unit. International Journal of Nursing Practice 11, 142-149.
- Gill, P., Stewart, K., Treasure, E., & Chadwick, B. (2008). Methods of data collection in qualitative research: interviews and focus groups. British Dental Journal, 204(6), 291- 295.
- Grove, S., Burns, N., & Gray, J. (2013). The practice of nursing research: Appraisal synthesis and generation of evidence (7th ed.). St. Louis, MO: Saunders Elsevier.
- Grove, N., & McIntosh, B. (2005). Communication for person centered planning. London, United Kingdom: Foundation for People with Learning Disabilities.
- Hayes, H., Parchman, M. L., & Howard, R. (2011). A logic model framework for evaluation and planning in a primary care practice-based research network (PBRN). Journal of the American Board of Family Medicine,24(5), 576-582
- Holburn, S., Jacobson, J. W., Schwartz, A. A., Flory, M. J., & Vietze, P. M. (2004). The Willowbrook futures project: A longitudinal analysis of person-centered planning. Journal Information, 109
- Holburn, S., & Vietze, P. (Eds.). (2002). Person-centered planning: Research, practice, and future directions. Paul H Brookes Pub
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, D.C: National Academy Press
- Jordan-Evans, S., & Kaye, B. (2002). Retaining employees. Bloomsbury (2002), Business: The Complete Guide, London: Bloomsbury, 196-197
- Kelly, D. (2013). Applying quality management in healthcare: A systems approach. Chicago, IL: Health Administration Press
- Kettner, P., Moroney, R., & Martin, L. (2013). Designing and managing programs: An effectiveness-based approach (4th ed.), Thousand Oaks, CA: Sage
- Kloppenbog, T. J., & Petrick, J. A. (1999). Meeting management and group character development. Journal of Managerial Issues, 11, 166-167.
- Langley, G. J., Nolan, K. M., Nolan, K., Norman, C., & Provost, L. (1996). The improvement guide: A practical guide to enhancing organizational performance. San Francisco, CA: John Wiley & Sons
- Maeng, D. D., Davis, D. E., Tomcavage, J., Graf, T. R., & Procopio, K. M. (2013). Improving patient experience by transforming primary care: evidence from Geisinger's patientcentered medical homes. Population health management, 16(3), 157-163.
- Maslow, K., Fazio, S., Ortigara, A., Kuhn, D., & Zeisel, J. (2013). From concept to practice: Training in person-centered care for people with dementia. Generations, 37(3), 100-10
- McCance, T., McCormack, B., & Dewing, J. (2011). An exploration of person-centeredness in practice. The Online Journal of Issues in Nursing, 16(2), 1.
- cCormack, B., Dewing. J., & McCance, T. (2011). Developing person-centered care: Addressing contextual challenges through practice development. OJIN: Online Journal of Issues in Nursing, 16(2). Retrieved from
- McCormack, B., Wright, J., Dewer, B., Harvey, G., & Ballantine, K. (2007). A realist synthesis of evidence relating to practice development: Interviews and synthesis of data. Practice Development in Health Care, 6(1), 56-75
- McCormack, B., & McCance, T. V. (2006). Development of a framework for person-centered nursing.56(5),472-9. PubMed PMID: 17078823
- McEwen, M., & Wills, E. M. (2014). Theoretical basis for nursing. Philadelphia, PA: Lippincott William & Wilkins.
- principles from complex environments. Mahwah, NJ: Lawrence Erlbaum Associates. Mead, N., & Bower, P. (2000). Patient-centeredness: A conceptual framework and review of the empirical literature. Social Science & Medicine, 51(7), 1087-1110.
- Nadin, P., Orr, M., & Meagher, J. (2013). Good practice guidelines for person-centered planning and goal setting for people with psychosocial disability. A Project Report for Disability Care. Australia
- Newhouse, R. P., Dearholt, S. L., Poe, S. S., Pugh, L. C., & White, K. M. (2007). Johns Hopkins nursing evidence-based practice model and guidelines. Sigma Theta Tau International Honor Society of Nursing
- O’Dea, N. A., de Chazal, P., Saltman, D. C., & Kidd, M. R. (2006). Running effective meetings: A primer for doctors. Postgraduate Medical Journal, 82(969), 454–461
- Parish, S. (2005). Deinstitutionalization in two states: The impact of advocacy, policy, and other social forces on services for people with developmental disabilities. Research and Practice for Persons with Severe Disabilities, 30, 219–231
- Patrick, D. L. (1997). Rethinking prevention for people with disabilities Part I: a conceptual model for promoting health. American Journal of Health Promotion, 11(4), 257-260
- Pender, N. J., Walker, S. N., Sechrist, K. R., & Frank-Stromborg, M. (1990). Predicting healthpromoting
- Planas, L. G. (2008). Intervention design, implementation, and evaluation. American Journal of Health-System Pharmacy, 65(19), 1854–1863.
- Polit, D. F., & Beck, C. T. (2004). Nursing Research: Principles and Methods (7th ed.) Philadelphia, PA: Lippincott, William, & Wilkins
- Porter, C., Hollenbeck, J. R., Ilgen, D. R., Ellis, A. P. J. & West, B. J. (2003). Backup behavior in teams: The role of personality and legitimacy of need. Journal of Applied Psychology, 88, 391-403.
- Reeves, S., MacMillan, K., & Van Soeren, M. (2010). Leadership of interprofessional health and social care teams: a socio‐historical analysis. Journal of nursing management, 18(3), 258-264. Robertson, J. M., Emerson, E., Hatton, C., Elliott, J., McIntosh, B., Swift, P, & Joyce, T. (2005). The impact of person centered planning. Lancaster, CA: Institute for Health Research,
- Rabin, B. A., & Brownson, R. C. (2017). Terminology for dissemination and implementation research. Dissemination and implementation research in health: Translating science to practice, 2, 19-45.
- Robinson, J. H., Callister, L. C., Berry, J. A., & Dearing, K. (2008). Patient-centered care and adherence: Definitions and applications to improve outcomes. Journal of the American Academy of Nurse Practitioners, 20(12), 600-607.
- Sanderson, H. (2002). A plan is not enough: Exploring the development of person centered teams. In S. Holburn & P. Vietze (Eds.), Person-centered planning: Research, practice, and future directions (pp. 97-126). Baltimore: Paul H Brookes.
- Scott, T., Mannion, R., Davies, H., & Marshall, M. (2003). The quantitative measurement of organizational culture in health care: A review of the available instruments. Health Services Research, 38(3), 923-945.
- Senge, P. (2006). The fifth discipline. London: Random House Business Books. Slater, P., McCormack, B., & Bunting, B. (2009), The development and pilot testing of an instrument to measure nurses’ working environment: The Nursing Context Index. Worldviews on Evidence-Based Nursing, 6, 173–182.
- Tondora, J., O'Connell, M., Miller, R., Dinzeo, T., Bellamy, C., Andres-Hyman, R., & Davidson, L. (2010). A clinical trial of peer-based culturally responsive person-centered care for psychosis for African Americans and Latinos. Clinical Trials. 7(4), 368-79.
- Viau-Guay, A., Bellemare, M., Feillou, I., Trudel, L., Desrosiers, J., & Robitaille, M. J. (2013). Personcentered care training in long-term care settings: Usefulness and facility of transfer into practice. Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 32(01), 57-72.
- Winter, J. K., (2000). Student evaluation of a learning exercise designed to develop effective meeting skills. Journal of Education for Business, 75, 210-215.
- Zamanzadeh, V., Ghahramanian, A., Rassouli, M., Abbaszadeh, A., Alavi-Majd, H., & Nikanfar, A.-R. (2015). Design and implementation content validity study: Development of an instrument for measuring Patient-Centered Communication. Journal of Caring Sciences, 4(2), 165–178
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



