Innovation in NHS for Better Outcomes
Introduction
Innovation is crucial in supporting NHS to achieve the ambition which has been set in the Mandate to bring a change and provide better outcomes to patients in all the five domains of NHS Outcomes Framework (NHS, 2018). National Health Service (NHS) faces massive challenges to improve quality of patient care while workload and financial pressures have been growing considerably. Quality improvement needs designing and redesigning work process that deliver better outcome and lower cost (The King’s Fund, 2018). Nurses are motivated to become involved and participate in innovative practices since they try to improve health outcomes, patient experiences and nursing practices. To develop and support the nurse-lead innovation, it must be clinically effective and acceptable to the patient. In addition, it must be demonstrated that limited healthcare resources are used (RCN, 2018).
Diabetes is a long-term condition and people who suffer from this condition have the right to experience good quality of life. Therefore, it is the healthcare professionals especially the nurses to develop partnership approach for improving the quality of diabetes care and support these in managing and improving the condition. Consequently, the condition demands efforts and sacrifices to change life style and cultural pattern. The patient service innovation in this dissertation aims to improve glycaemic control by dietary education in British South Asian s (BSA) individuals who suffer from diabetes. This minority group has limited access to education centres and services due to poor education, language barrier, cultural inhibitions and other factors. Coates and Flannery (2010) outline, BSA individuals are at high risk of developing T2DM. They have up to five times greater chance of having the disease than the European populace. NHS (2018) outlines, around 9 out of 10 individuals with diabetes have T2DM and one of the main factors is poor diet. Therefore, structuring education programmes for adults with diabetes is covered by NICE quality standard (NICE, 2018).
At the beginning of this dissertation, the recent challenges of the NHS with key development points, polices, drivers, NHS Constitution, The NHS Five Years Forward View (FYFV) and NHS Framework will be summarised briefly. Following this, the background of the chosen subject which has raised the rational and aim of the objectives of PSI, related evidences as NICE and other clinical guidelines and recommendation will be discussed. Next, the rational of the chosen innovation and how it can address the area of concern, patient benefit and service innovation improvement, have been outlined. The second part includes the plan, implementation of the change and evaluation of the chosen PSI as well as the leadership theory. Finally, the conclusion will review the main points and conclude the dissertation.
Theory
The health secretary Aneurin Bevan launched the NHS first time in 1948 to bring hospitals, doctors, pharmacists, nurses, dentists and opticians under one organisational umbrella , providing free services at the point of delivery regardless of wealth which is the core principle. NHS establishment gives the opportunity to the poor who did not have the access to the treatment while the service care has remained the same as before (NHS, 2018). In the last 70 years, NHS has transformed the health and wellbeing of the patient, delivered massive medical advances and helped the public to live longer (NHS, 2018). According to the King’s Fund (2018) NHS has been under severe pressure which has increased recently. The reasons for the pressure are financial, political and social. The aging population, the growing population, obesity, diabetes, antibiotic resistance, cost of medical technology, centralisation drives and increase of reliance on private services are the main challenges NHS has faced. 1.6 billion pounds were provided for the NHS that can cover the NHS funding growth to 2.4 per cent which is higher than 2 per cent in 2017/2018 but still lower than the 4 per cent average of NHS. 10% of this budget is spent on diabetes (Diabetes UK, 2018). NHS belongs to the nation and wants to improve the population health and wellbeing mentally and physically. NHS is founded based on principles and values which bind the communities, patients, public and staff altogether. The NHS Constitution is consisted of the NHS of England’s principles and values. It clears the public, patient and staff’s rights entitlement, NHS’s commitment for achievement, responsibilities of the public, patient and staff to each other to make sure NHS is operating effectively and fairly. The NHS is guided by the seven key principles and core NHS values which are directed by the staff, patient and public’s discussion. The NHS values deliver common ground for co-operation to accomplish shared aspirations at all level of the organisation under consideration. Everyone using NHS has a legal right which is summarised in constitution and written in detail in the Handbook to the NHS Constitution. NHS Constitution outlines that NHS has social duty to promote equality and if the health improvement in a group does not keep pace with the rest of the population, it should be supported and offered help (NHS, 2015). Therefore, the BSA minorities should be supported to improve their condition. Referring to England (2018), the FYFV outlines how and why NHS should be changed. Mainly a health gap, quality gap and financial sustainability gap are the frameworks which are to be improved. The triple aims of better health, better care and better value are why the improvement is needed. Action on prevention has been taking place including cigarettes plain packaging, diabetes prevention programmes, sugar tax, meningitis and flue vaccination and public health campaign such as ‘’ Be Clear on Cancer’’ and ‘’Act Fast’’. The Department of Health and Social Care developed set of indicators called NHS Outcomes Framework to monitor the adult and children’s health outcomes in England. This is an overview of how NHS is performing. The NHS Outcome Framework consists of five significant domains and aims to improve health of the population and reduce health inequalities. The most relevant domain of NHS Outcome Framework for this innovation is domain 2, Enhancing Quality of Life for People with Long-term Condition. The indicators analyse the results of the surveys to measure individuals’ quality of lives which are based on people’s experiences in primary care (NHS. UK, 2018). Improving the quality of life of these individuals needs dietary education. All the polices, values, strategies and recommendations are set to improve and move NHS into the future, provide high quality care for the nation while using less services at lower costs. Another significant part of health system is clinical governance that covers activities that maintain and improve patient care with high standard such as quality and safety improvement. Health care organisations are accountable to provide these activities to communities and upheld the standards of these. In addition to the safety and quality of the patient care process, dealing with complex problems, taking new approaches for good clinical practice and making sure that lessons are learnt from the failures are its responsibilities (Scally and Donaldson, 1998). Diabetes UK through Diabetes Watch assesses and monitors services delivery in different areas of health care and Diabetes Voice pushes service improvement by influencing and campaigning (Diabetes UK, 2018). Consequently, leadership is a great influential aspect to shape the culture of the organisations, ensuring the required leadership behaviours and improve the qualities of care (The King’s Fund, 2015). The 6 Cs: Competence, Care, Compassion, Commitment, Courage and Communication are vital element in nursing practice. These values are the primary components of Leading Change Adding Values framework. The framework is for Midwives, nurses and care staff, where they work and no matter what their roles are. This framework is founded on compassion in practice and is directly allied with the FYFV in similar working on person-focused and providing unified care across the boundary separating health and social care traditionally. It aims at the triple targets: health and wellbeing, care and quality and funding and efficiency. The framework includes ten commitments and the second commitment of this framework promises to increase the visibility of midwifery and nursing in leadership and making input in the prevention of ailments (NHS, 2018). Following Frances inquiry (2013) and the recommendation, the necessity of empowering the nursing leaders has been highlighted. Moreover, the Berwick report (2013) addressed the main problems affecting patient safety in NHS and made recommendations (GOV. UK, 2018). The shape of caring review carried out by Health Education England (HEE) and Nursing and Midwifery Council NMC (2016) recommended that nurses and healthcare staff at any level are needed to support, lead innovation and research in providing high quality care (RCN, 2016). Overall the reports and recommendations require changes and the changes need good leadership to achieve the goals and overcome the challenging obstacles where nurses play crucial part in leading and managing.
Continue your exploration of Foodborne Illnesses: Causes and Impact with our related content.
The nurses need the required knowledge and skills to be able to lead, challenge, implement and evaluate for service improvement. Health innovators must ensure that the patient is at the centre of everything they do. This is the core principle of NHS constitution (Tailor, 2017). This patient service innovation intends for a change for service improvement in clinical conditions, patient experience, communication effectiveness and learning effectiveness which require team working, effective communication between healthcare professionals and good leadership.
Background
NICE (2015) defined T2DM as a chronic metabolic condition either caused by insulin resistant or insufficient production of it by pancreas. NHS spends 8.8 billion only on T2DM each year. This condition causes up to 23 limb amputations in a day in UK. Approximately 22000 individuals with this condition die early every year (England, 2018). It is the fastest growing health threat. Approximately over 4 million individuals living in UK suffer from this condition whereas in every 16 person one is diabetic. Diabetes is a long-term condition which has a sever health complications, however the premature death can be prevented by minimising the main complications (Diabetes.UK,2018). Having poor glycaemic control causes severe vascular complications as well as impairment of vital organs such as heart, kidney, liver and eyes. These individuals have up to two times higher risk of death from heart diseases and up to four times higher risk of death from stroke. In addition, life expectancy is up to 10 years less with this condition and these individuals are at high risk of death from heart diseases and stroke (Diabetes.UK, 2018). T2DM is up to six times more common in African-Caribbean and South Asian origin referring to the South Asian community generally limited to Indian, Pakistani and Bangladeshi decent who together are the largest minority in UK. Experts believe that diet, lifestyle and storing fat in the body are the major cause in this ethnic group (Diabetes UK, 2018). Hence, a culturally sensitive multi-disciplinary approach for management of diabetes in immigrant population is needed (Venkatesh et al., 2012). Hence, nutrition is a great contributor in enhancement of the T2DM especially glycaemic control. It is part of the treatment and balancing of the right amount of the micronutrients and macronutrients contributions to have a healthy life-style. However, medication plays a vital role in management of this condition but having a healthy and balanced diet is as important as the medication (Diabetes.UK, 2018). Dietary advice and guidelines aim not only to ensure the adequacy and prevention of deficiency but also prevent or delay the onset of most of the diseases (Webb, 2011). Diabetes diet is the vital part of the treatment and it contains two main parts, what should be eaten and how much is the right portion. A dietary reference value outlines upper and lower amount of nutrients to prevent deficiency and toxicity which can be used to measure and design food supply for a specific group or population. It is more beneficial for people who could be attributed to the possibility of risks regarding getting affected by diseases (Fox et al., n.d.) The main cause of obesity and insulin resistance is diet rich in saturated fat which also elevates the circulation of free fat in the blood. Reducing saturated fat intake can help to lessen the need for the excess insulin (FACLM, 2017). Another research (Venkatesh et al., 2012) revealed that lack of alteration of Asian traditional high carbohydrate and fat to a healthy diet could be the cultural causes of high HbA1c level. Diabetes patients form major sub-section of the society and the needs are different in each person therefore the dietary education should be tailored individually according to their requirements. The condition has a deep psychological effect on affected individuals and causes their poor quality of life. This is, in turn, associated with weak adherence to treatment and increase mortality and morbidity rate. The process of listening to the patient’s experience of suffering could help the health professionals to be more genuine. It is necessary to have access to their world of emotions, feelings, their social milieu and experiences and how the advanced technology has impacted on their lives (Isla, 2011). BSA decent is up to six times at high risk of developing T2DM than the Europeans. In fact, these individuals make up 4% of UK population but 8% of the UK diagnosed diabetes cases (Diabetes.UK, 2018). The high incidence of this condition has a significant ramification in this group whereas they have 2-4 times higher risk of stroke and myocardial infarction. It is estimated that by 2030 there will be 120.9 million people having diabetes in South Asia whereas 90-95 percent of the cases will be related T2DM. This figure is more than double of cases in Europe and North America. The BSA populations have higher prevalence of T2DM than the other ethnic groups (Gujral et al., 2013). T2DM in young South Asian individuals lead to higher risk of heart disease and many other diseases than the whites. This minority group with T2DM aged 20 to 60 are at high risk of cardiovascular problems and related conditions such as heart attacks, high blood pressure and high cholesterol and the rate of survival is very low in this decent group. In addition, in this community, people are at risk of T2DM from the age of 25 whereas the estimated starting age is 40 at white population. While this condition is very serious but if these are not diagnosed in the proper manner, then these could persist for up to 10 years.

Contrary, it appears genetic composition plays a significant part as well as modifiable lifestyle factors. More researches and investigation are required to be done to find the factors affecting and understand the differences (UK, disease and possible, 2018). Insulin resistance is more common in South Asian communities than Caucasians even at younger age and at comparative BMI. The reason for this tendency appears to be the accumulation of visceral and abdominal fat. It has been found that even in non-diabetic South Asian populace, the excessive visceral fat is accompanying increased insulin intolerance (Gujral et al., 2013). Even with diabetes programmes and guidelines for improving diabetes management, control of diabetes remains at the lower standards in many populations including the South Asians (Gujral et al., 2013). Lack of knowledge and health control in this group makes behavioural modification difficult (Lucas, Murray and Kinra, 2013). The clinical review shows that education intervention in South Asian population who are socio-educationally deprived can be well received by using community-based programmes with experienced bilingual community workers in a familiar environment (Chapman, Qureshi and Kai, 2013). Sohal et al (2015) systematically reviewed s in South Asian patients and had outlined that language and communication discordance with heath care professionals was the main reason of issues receiving and understanding diabetes education. The reason for adopting a diabetes diet was due to lack of sufficient details, misconception on the element of diabetic diet and social burden to continue consuming traditional diet. Therefore, the diabetes programmes focusing on communication improvement, addressing predominant misconceptions and specific cultural approaches had been needed for this group.
Rationale/ Aims
The aim of this Patient Service Innovation is to improve glycaemic control in BSA population by dietary education through education sessions and leaflets in their own languages. Mainly the intervention is meant to increase the quality of life (Domain 2 of NHS Outcome Framework) of these minorities group. In addition, it is beneficial for NHS that it could reduce its cost spending on diabetes complications. Bhurje et al (2016) clinical trial revealed reduction of glycated haemoglobin (HbA1c), fasting blood lipid, blood pressure, life style modification and treatment, decreases cardio vascular complications and the associated rate of mortality by 57% per cent, mortality by up 46%. Tailored intervention using diet management tool significantly improve glycaemic control in T2DM patients (Shamsudin et al., 2016). Another study (Misra A, 2018) discovered, national community intervention programmes based on creation of awareness regarding the consequences of consuming unhealthy food and replacement of it with healthy food are needed for populations in South Asian countries and South Asian migrant communities. Diabetes programmes and various national guideline bodies recommend diabetes education, behaviour change for promoting diet, exercise and medication adherence to achieve reducing HbA1c, lipids and blood pressures. Also, as the cultural belief among BSA individuals have an important effect on their behaviour toward diabetes therefore understanding of their culture is valuable for improvement of care delivery in the community (Nursing Times, 2012). Intervention targeted the Asian Indian communities having T2DM must include specific cultural adaptation to nutrition education (Venkatesh et al., 2012). NICE (2011) recommended, structured education programmes aid adults with T2DM to improve their skills and understanding of the condition, in motivating them to control the conditions and manage them effectively.
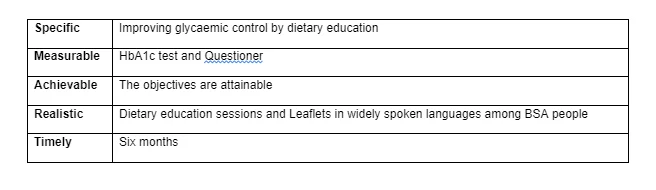
The SMART objectives are set to outline the chosen innovation clearly.
Lim et al (2009) revealed nutrition education is effective in obedience to diet recommendation and improving glycaemic control. BSA people with T2DM require tailored education for better understanding of their condition. Checking their level of understanding and finding their learning needs will help them to improve self-management effectively (Sunsoa, 2015). The positive change on healthy food intake in this population will improve their glycaemic control which prevents most of the complications of this disease. Obtaining six-month HbA1c outcomes in intensive education programme and conventional education indicate that structured and systematic guidelines can improve diabetic patients’ biomedical outcomes compared to unstructured ones. The structured education led by nurses and health educators has the potential to improve diabetes management and reduces the complications (Essien et al., 2017). The Root Cause Analysis (RCA) through five whys have been used to identify the service innovation improvement by causative factors leading to the need of this PSI. The South Asian individuals with diabetes and community service are involved in this process. The fish tail analysis (Appendix 1) will summarise the main factors. The simple technique is to ask the question why, to get the root cause.

The project plan:
Change management strategy
Implementation of change in organisations is the main part of nursing leadership competency as well as a daunting responsibility. Models of change help nurses to avoid change fatigue and motivate them to move toward safer system of care (Reineck, 2007). The change models are used as a framework for any programme or project which could require transformational change, sustainable change and aims to deliver real benefits for patients and public. Importantly, it supports health and care adopting a shared approach to transformation and leading change (England, 2018). According to Nursing theory.org (2018), Kurt Lewin has developed “The Changed Theory of Nursing which is his most influential theory”. The three- stages model of change acknowledged as Unfreezing- Change-Refreeze model was theorized by him. In unfreezing process, the old pattern can be changed to overcome the strains of individual and group traditionalism. The change stage involves thought, behaviour and feeling changes. The last stage, refreezing, is the establishment of the change as the new habit which is very important as the patient can go back to his habit easily without this stage. Brisson-Bank (2010) summarised, Kotter brought together the change models and transition into eight steps which should be followed in correct order and correct way. Kotters 8 steps is summarised in three main parts that are, creating the climate for change, engaging and enabling the change and implementation with sustaining the change. Status Guides (2018) outlines, the ADKAR model was developed by Jeff Hiatt which not only focuses on sets of steps, however, the leader should try to hit a group of goals. It includes awareness, desire, knowledge, ability and reinforcement. The main focuses on this model is helping employees to understand, interact and carry out changes. Since the model is focusing on goals, the leader can easily take it and adapt it to the organisation’s structure and culture. Conversely, if the leader wants a macro-level change and is unaware of how deep the transition can go this method is not probably the required one. Moreover, McKinsey 7S Model is more holistic as it requires deep analysis of all parts of the organisation by leaders. It offers different ways for change, but the significant disadvantage is that if a part of the plan fails, it affects other areas as well. Implementation of the change faces numerous obstacles but using the framework helps to overcome some of potential barriers. In contrast, the success is not granted and at every stage the changes can be vulnerable to failure in all of the change theories (Mitchell, 2013). Different theories can be used according to specific circumstances of the environment. The chosen model for this PSI is Lewin’s Change Management Model since visual language is provided excellently for leaders to take action. It is practical and offers a high-level approach for change. It helps and supports the leaders to follow three main steps including making a radical change, minimising the disruption and making sure the change is sustainable (Morrison,2014). However, the model did not offer the ways dealing with people who are resistant to changes (Status Guides, 2018). Initially, for unfreezing stage patient motivation and encouragement are crucial. As the major component of the project is improving glycaemic control in BSA minorities by dietary education, this group should be assured that extra lingual help can be offered. Mainly, a deep understanding of the barriers and what is needed to be achieved should be considered to have a significant outcome. Open discussions are required to identify if change is beneficial for patients and the healthcare staff (Stephenson, Mitchell and Mitchell, 2011). Barriers for diabetic diet adoption is mostly lack of enough detail on BSA tailored diet, misunderstanding on the component of the diabetes diet, lack of knowledge and continuing with a traditional diet due to the social responsibilities. Sohal et al (2015) revealed that lack of time with health care workers and reassurance from the health professionals, lack of awareness on quantity and component of the diet and language discordance are significant barriers to diabetes management. First, the MDT meeting should be organised to have a shared decision making on how and where the education session can be placed. Involving patients in the preparation of the sessions and leaflet is necessary to find out what they want to be included. Moreover, inviting the interpreters and bilingual healthcare staff to help with the sessions are necessary. All of the members of the team should be trained and have the competency delivering content of the programme. The content of the programme is theory-driven, evidence based and comprehensible which could be measured and reviewed by independent and trained personnel for assurance and consistency. For the innovation to be successful, the cultural, literacy related, cognitive, linguistic and traditional aspects related to the dietary conditions are needed to be considered carefully. It is recommended that people from ethnic minority groups should be offered culturally sensitive multi-component education and intervention (Dyson et al., 2018). Accordingly, dietary education needs to be centred on the example of traditional food of BSA people and ingredients. To improve the diabetes targets, the implementation of culturally tailored education programme is necessary. Also, the season should be relied on bicultural and bilingual health information as well as deep understanding of the cultural belief and sensitivity to improve diabetes management. Change is the moving stage of Lewin model. The dietary education consists of education sessions and leaflet distribution mainly in most spoken languages (Panjabi, Urdu, Bengali, Hindi, Sanskrit and other languages) among this group. During this process, the sessions will mainly take place in a local GP Practice and can be organised in a library, masque, church, temple or any other patient preferred place which could be available. The Multi-Disciplinary Team (MDT) across primary and secondary care including community and general practice services are actively involved in diabetes care pathway. The trained community health care professionals with the support of dieticians and diabetes specialists will be involved in the process. Practice nurse has the main role in this project. Patients who could fulfil the inclusion and exclusion standards will be allocated in three different groups. Bashir et al (2016) report revealed that flyers were being more reliable and up to date than websites. For some of the patients, leaflets have made a big change in management of the condition and their understanding about the conditions as well. Many participants preferred face to face contact with health educators. Because, in this valued method they can ask questions, get personalised and tailored advice and seek clarification. Consequently, addressing the language barriers, it is necessary that the leaflet should be available in different languages. The information in the leaflet should be approved by dieticians since, Diabetes UK (2018) outlines the diet should be based on principle of healthy eating focusing on food that do not affect blood glucose level adversely. The NHS and Diabetes UK recommend a balanced and healthy diet that includes high level of fresh fruit and vegetable and low in fat, sugar and salt (Diabetes UK, 2018). The diabetes diet has moved from a calorie- restricted diet prescribed by physicians towards the individualised meal plan which considers the preferences of the individuals and dislikes and cultural background (Burke, Sherr and Lipman, 2014).
The refreezing is the final step and the MDT is responsible to make sure that the change is sustainable. The continuous education programme will ensure the permanency of the change.
Leadership theory
Leadership is not only the understanding of the processes and systems, it is an adaptability skill to think differently to bring a change, copping today’s challenges and being part of the future. There is a robust relationship between the leadership and high-quality care as well as compassionate care (Cummings and Cummings, 2014). Leadership is a significant influential aspect in shaping culture of the organisations, ensuring the essential leadership behaviour and developing the qualities of care (The King’s Fund, 2015). Henwood (2014) outlined, leadership cannot be the accountability of a person but as a contextualised process needs collaboration to deliver excellent outcomes. Therefore, it is the responsibility of all of the staff to collaborate however they may not have the formal role. Multidisciplinary primary care team plays a crucial role in prevention and management of diabetes within their competencies. Specialist teams comprise physicians, nurses, dieticians, paediatricians and clinical psychologists. They also have facilitating and coordinating roles such as education, training and surveillance for complications (Diabetes UK, 2018). The team effectiveness is greatly influenced by combining the expertise and strengths to enhance comprehensive patient care delivery systems(Wolfsdorf, 2012) . Teams that include diabetes educator can offer education, improve quality of life, glycaemic control and reduce risk of complication as well as healthcare cost (Siminerio, 2015). The Interdisciplinary Team (IDT) approach is very effective in delivering care to individuals who have T2DM and thus require great life style alteration and management. The IDT based care delivering glycaemic control improvement and reduction in HbA1c level. The focus is on specialists in the team to work collaboratively rather than alongside each other and flexibility is needed with respect to professional boundaries. Therefore, a supportive and strong leadership is necessary for successful delivery. It should be clear that when and how to start the project and the team composition should be based on local needs, clinical setting and available resources (McGill et al., 2017). The fundamental characteristics required for a healthy culture are: inspiring values and vision, having goals and performance, compassion and support, learning and innovation, good team working and collective leadership. Leaders must communicate an inspiring, ambitious vision and forward-looking focused strategy at every level to offer high-quality and compassionate care to the communities they are working for (The King’s Fund, 2018). All nurses perform as agents of change, driving policy and processes and leveraging technology to provide better and affordable care for individuals as well as the community (Nursingworld.org, 2018). NICE (2012) recommended, development of patient’s understanding should be individual as well as how the patient is affected by the condition and how the person’s experience and circumstances affect the treatment and condition. Effective and open communication and shared management goal within the team has great impact on care outcomes. The leader of this PSI should convince the MDT and patients to adopt dietary education as the main aspect of improving glycaemic control. The most recent evidence-based and comprehensive information must be given to the group for an effective outcome. Now diabetes specialists believe that metabolic control is important and the role of dieticians go beyond the identification of the meal plan and this involves working with patient to design meal algorithms, negotiate dietary strategies, provide tailored programmes based on patients’ needs and lifestyle modification (Journal. Diabetes. org, 2018). Accordingly, to convince this minority group, dietary education needs to be centred on example of traditional food of South Asian communities and their ingredients. To improve the diabetes targets, the implementation of culturally tailored education programs is necessary. Also, the session should be relied on bicultural and bilingual health information as well as deep understanding of the cultural beliefs and sensitivity to improve diabetes management (Sohal et al., 2015). Dietary education increases patient’s awareness resulting in better focus of control which improves their sense of self efficacy. The strong self-esteem helps them to recover from negative emotions . In contrast to this, low self-esteem causes poor reaction towards negative emotions and makes them vulnerable to threat and they need protection.

Time management
The predicted time for making the plan, implementation and evaluation of the chosen PSI is approximately six months. To accomplish goals efficiently, this PSI needs a careful and practical time management. Meanwhile any unexpected interruption may happen that can delay the project. Scheduling the extra time for occurrence of any unexpected one will prevent the project being delayed. Good planning will improve the effectiveness of the outcome. Time management is very important since time cannot be saved for later utilisation. You can approach what you desire by management of time wisely. It will help to set up the priorities, enable you to be more creative and proactive that helps to do the right things at the right time (Sasson, 2018). This PSI needs an appropriate time management to be effective and successful. Planning, setting the goals, delegation of MDT, listing the priorities step by step and completing each section on the right time will contribute in the value of the outcome significantly. On the other hand, the poor time management will cost NHS as well. The GANTT chart (Appendix 2) outlines the time management of this PSI from the beginning to the end.
Evaluation
Any change within the health care organisations need to be quality assured and according to the clinical excellence framework to deliver exceptional care. Quality assurance in the NHS involves three main components which are Patient Safety, Patient Experience and Clinical Effectiveness. In the primary care, Significant Event Audits are undertaken to take a lesson from any untoward event which could have happened. The aim of the safeguarding professionals is to ensure that commission services protect people’s rights, independence and well-being. In addition, they secure assurance that those individuals being at risk stay safe, ensuring they are safeguarded against neglect, abuse, embarrassment, discrimination and poor treatment (NHS, 2018). The result of an evaluation of an innovation should be above the level of satisfactory and decisively to cover clinical excellence . Any change requires evaluation to determine improvement of the standard which can be done by patient satisfaction survey and clinical audit (Mitchell, 2013). Patient satisfactory survey as a realistic tool has been used for quality improvement in healthcare industry. It is a vital and meaningful source of information, to find the gap and develop an effective action plan, for healthcare organisational’ structure improvement in an according manner. Patients’ evaluation of care delivery highlight opportunity improvement, develops decision making strategies, lessens costs, frames effective management strategies, meet expectation, monitors performance of healthcare industries and provides benchmarking across healthcare organisations (Al-Abri and Albalushi,2014). The aspects of evaluation for this PSI have two significant parts. First, the pre and post questioners (Appendix 1) will be used to find out the level of South Asian individuals’ knowledge regarding the condition and diet. The primary step for developing an education plan is to obtain information regarding patient current knowledge, behaviour, skill and attitudes to plan appropriate teaching approaches to the patient (Wolfsdorf, 2012). The questions before the implementation and after the implementation will be the same to better clarification of the enhancement. Second, the Haemoglobin A1c (HbA1c) will be measured to evaluate any improvement in long-term glycaemic control. In addition, raising awareness to keep the glycaemic control within the target goal has a positive impact on these individuals. For patient with T2DM the HbA1c target is 48mmol/mol which is 6.5% however the doctor may suggest different target for different people (Nice, 2015). The measurement of both the improvement of level of knowledge and glycaemic control will identify the successfulness of the PSI. The outcome will be sustainable by continuous and active contribution of the MDT involving not only in this process but any action which improve health promotion, raising awareness that food influences health, improving education of those who are affected the most and better understanding of the fast growing multicultural and multilingual society.
Role of the nurse in PSI
The process of researching on theories, policies, guidelines and writing the PSI itself had a great impact on knowledge and understanding of the project development . During the progression of the innovation, many crucial aspects of nursing such as, critical thinking, coordination, advocacy, delegation skills and knowledge of the subject will be improved positively. This experience and responsiveness will provide the opportunity to contribute in fight against diabetes. Diabetes, especially T2DM is the major challenge of NHS and the culture and community requirement aid to have more facilities and effective programmes. Concerning this project, plan implementation and evaluation of it certainly enhance the knowledge of the inventor and boost the confidence to take part in similar intervention in future. Through the experience the major affecting challenges has been identified and significant evidences and statistics has been acknowledged on the most vulnerable populations. The professional transformation happens through knowledge and skill development and working in collaboration with MDT, community and patient. Understanding people’s culture and how their individuality is related to their culture is very important for nurses. This will ease the communication and understanding of people with different background and culture. In addition, Culture should not be a barrier to individualistic care and health education and people can develop their understanding. Moreover, it is crucial to consider that the information given to the patients could be understood and has been interpreted in a cultural context accurately (Nursing times, 2012). Since, there is not enough dietician and nutritionists in healthcare industry, nurses fill the role of dietician counsellors. However, they do not obtain extensive education in nutrition they use the opportunity as researcher or educator (Henning, 2009). Nurses ensure that nutritional needs of the patients are met, giving nutrition advice and provide nutrition screening for patient’s healthy eating improvement and better health outcome (Bennett and Duffy, 2007). Decent cooperation between the nurses and dieticians is fundamental for achievement in patients’ health. Diabetes educator provides the required self-management education and community health workers coordinate care and support patient in behaviour change for better health outcome (Siminerio, 2015). Quality in the healthcare system is a multidimensional framework that includes six domains such as effectiveness, efficiency, equality, safety, timeliness and patient-centeredness. Finding the relationship of the various factors affecting quality in the patient pathway not just informed decision making progression in aiming the interventions but it will help to sustain patients’ high-level quality care in the NHS for future (Friebel, 2017). In the increasingly competitive health care environment, healthcare mangers are weeded to focus more on excellent rating of patient satisfaction through improving quality of service delivery. Therefore, factors influencing patient satisfaction are used as a mean to measure the quality of healthcare delivery. The demographic factors such as age, gender, education and health status affect patient satisfaction. Patient satisfaction is identified as an important indicator of quality outcome where the success of the service delivery system can be measured greatly. Role of the nurse as a leader in this PSI is to improve patient care in the community and implementation of evidence into practice. The goal is to change nursing culture and involve the patients who are vulnerable and need more support for a shared decision making with collaboration of MDT. The main roles of the nurse as a project leader are planning the project, listing all the activities for carrying out the project, addressing the patient affecting factors in an appropriate action plan, considering cost effect, time management and ensuring the safety and ensuring the quality of the mission.
Conclusion
To conclude this PSI, identifying the main factors causing unhealthy choices significantly aids the plan, implementation and evaluation of the dietary education for improving glycaemic control in South Asian individuals living in UK. Patients should be motivated that medication is not the core option to reach better glycaemic control. Consideration of quality of food, consumption of good nutrients and better management improve the glycaemic control as well as the quality of life. The key themes to apply to this project in the community are education which raise awareness and improve behaviour change. Consequently, patients’ willingness to improve their glycaemic control will be increased. Focusing on the main reasons help the researchers to develop comprehensive action plans accordingly. Lack of understanding of this long-term condition and its complications, generally lead to inadequate glycaemic control. Moreover, an effective leadership prove a safe and collaborative environment and high-quality care which ease the project process. Also, a decent leadership will help to have the right decision that is beneficial for both the staff and patient. Nurses are the main member of MDT in the community, overcoming challenging situation, working hard to bring changes for the best interest of the patients, NHS and society. Implementation of an innovation requires comprehensive knowledge of the theories, polices, guidelines, recommendations as well as challenges, understanding of patients’ beliefs and preferences increase the innovation developers’ awareness to predict the consequences in the process. As a result, dietary education empowers the patients to improve their conditions, increases the value of their lives and helps them to reach their full potential. Working as a team with the other healthcare professionals will bring a significant change which could be needed for the rapidly changing health society.
References:
- Al-Abri, R. and Al-Balushi, A. (2014). Patient Satisfaction Survey as a Tool Towards Quality Improvement. Oman Medical Journal, 29(1), pp.3-7.
- Bashir, N., Dayson, C., Ismail, M., McCarthy, L. and Chowbey, P. (2016). Making the most of primary and community services: what works for BAME people with long-term conditions?
- Chapman, J., Qureshi, N. and Kai, J. (2013). Effectiveness of physical activity and dietary interventions in South Asian populations: a systematic review. British Journal of General Practice, 63(607), pp.e104-e114.
- Dyson, P., Twenefour, D., Breen, C., Duncan, A., Elvin, E., Goff, L., Hill, A., Kalsi, P., Marsland, N., McArdle, P., Mellor, D., Oliver, L. and Watson, K. (2018). Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabetic Medicine, 35(5), pp.541-547.
- Essien, O., Otu, A., Umoh, V., Enang, O., Hicks, J. and Walley, J. (2017). Intensive Patient Education Improves Glycaemic Control in Diabetes Compared to Conventional Education: A Randomised Controlled Trial in a Nigerian Tertiary Care Hospital. PLOS ONE, 12(1), p.e0168835.
- Gujral, U., Pradeepa, R., Weber, M., Narayan, K. and Mohan, V. (2013). Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Annals of
- McGill, M., Blonde, L., Chan, J., Khunti, K., Lavalle, F. and Bailey, C. (2017). The interdisciplinary team in type 2 diabetes management: Challenges and best practice solutions from real-world scenarios. Journal of Clinical & Translational Endocrinology, 7, pp.21-27.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



