Dysphagia in Post-Stroke Patients
Chapter 1: Introduction
1.0 Introduction
The World Health Organisation refers that stroke is a form of clinical syndrome which is presumed to be vascular in origin that is typified by rapid development of signs of global or focal disturbance related to cerebral functioning which lasts more than 24 hours or may lead to death (Coupland et al. 2017). In post-stroke patients, malnutrition is most prevalent hindrance faced by them. This is because after stroke dysphagia is of the common clinical consequence faced by them. Dysphagia involves difficulty of the post-stroke patients in pharyngeal and oral phases of swallowing food and increasing risk for complication in respiration (Steele et al. 2016). This means that the post-stroke patients experience hindrances in swallowing food, as a result, they reduce their food as well as fluid intake. It results the patients to face malnutrition along with dehydration because proper amount of nutritious food is not taken by them. The further incidence of malnutrition occurs in post-stroke patients because many nurses are found to lack effective training and knowledge regarding the way they are going to tackle the clinical condition of dysphagia which leads to malnutrition among the patients. This result in making the nurses feel confused regarding the way they are to play their care role in effectively supporting post-stroke patients so that malnutrition among them is prevented or resolved. Thus, to identify the role of nurses to prevent malnutrition among post-stroke patients the study has been framed.
Looking for further insights on Enhancing Organisational Efficiency? Click here.
1.1 Research Rationale
The stroke is one of the leading causes of disability and death among UK individuals. In the study of Townsend et al (2012), it is informed that in the UK on a yearly basis 150,000 people experience stroke. In England, it is reported that 32,000 deaths occurred due to stroke-related issues (www.stroke.org.uk, 2012). Thus, it can be regarded that stroke is one of the key health issues in the UK. Moreover, it is informed that 6-62% of individuals post-stroke face the issue of malnutrition (www.bda.uk.com, 2013). In a recent study by Gomes et al. (2014), it is identified that in the UK the prevalence of increased risk of malnutrition in hyperactive stroke patients is 29%. The study by Sura et al. (2012) further informed that the cause of the increased risk of malnutrition is dysphagia among the individuals. This is because dysphagia results the individuals to experience difficulty in swallowing food and the patients to avoid pain with swallowing of food refrains to maintain proper intake of food. The issue of malnutrition among post-stroke has become a problem because it has lead to poor dietary intake resulting in increased incidences of disability, death and chest infection along with longer hospital stay (Gomes et al. 2014). The malnourished post-stroke patients also face issues with loss of weight leading to their physical inability to fight diseases. In the study of Çoban (2018), it is found that post-stroke men who are malnourished showed increased loss of lean mass compared to fat mass in comparison to women. Thus, this study also revealed that men are more susceptible to malnutrition than women in post-stroke condition. The malnutrition among post-stroke patients has become an issue now. This is because their malnourished state is making them prevalent in further complication such as pressure ulcers, falls, infection and others (Arsava et al. 2018). The rate of increased health complication is faced by post-stroke patients now as a result of malnutrition is due to fact that lack of nutrients is making the body’s immune system to perform ineffectively. This is because the energy required by the body to improve their body’s immune system and to face against infections is not present due to lack of effective nutrients. Thus, this study is required because it is going to shed light on the role of nurses which they require to perform to prevent malnutrition among post-stroke patients. This is because it would lead to better health status of post-stroke patients thus helping them to recover from the deteriorated health in an effective way.
1.2 Research Aim
The aim of the study is to identify the role of nurses in preventing malnutrition among post-stroke patients to improve their health.
1.3 Research Objectives
To identify the impact of malnutrition among post-stroke patients
To analyse the role of nurses in preventing malnutrition among post-stroke patients
To evaluate the challenges faced by nurses in preventing malnutrition among post-stroke patients
To suggest ways in which nurses are to prevent malnutrition among post-stroke patients
1.4 Research Questions
What is the impact of malnutrition among post-stroke patients?
What are the roles of nurses in preventing malnutrition among post-stroke patients?
What are the challenges faced by nurses in preventing malnutrition among post-stroke patients?
How are the nurses going to preventing malnutrition among post-stroke patients?

Chapter 2: Literature Review
2.0 Concept of Malnutrition
Malnutrition is referred to the condition which happens when deficiency to take in or utilise key nutrients for maintaining tissues growth and repair is not achieved that negatively impact on the individual’s mood, behaviour, physical health and other body functions. The malnutrition is often characterised by two or more of the factors such as weight loss, low energy intake, localised accumulation of fluid, loss of subcutaneous fat or decreased activity status (van Tonder et al. 2017). This occurs when adequate calories, protein, calcium and other nutrients essential for maintaining tissue function, growth and others are not effectively utilised. According to Malone and Hamilton (2013), acute or chronic diseases and starvation are often the results of malnutrition among adults.
2.1 Impact of Malnutrition
The impact of malnutrition on the adult or any other individuals is entirely negative. As mentioned by Correia et al. (2016), malnutrition results the individuals to face hindrances in making proper coordination with muscles and bones to maintain proper mobility. This is because lack of nutrients such as vitamin D, calcium, protein and others result the individuals to be unable to rebuild muscle strength in maintaining proper mobility. As argued by Mangus et al. (2017), malnutrition results in making organ failure to effectively execute their normal functioning. This is because the nutrient deficiency in the body leads to the loss of neurons in the body which are not replaced in proper amount for restoring effective functioning.
2.2 Risk factors for Malnutrition
Various factors are responsible for developing malnutrition among individuals such as chronic disease, depression, financial issues, dysphagia, overly restrictive diets and others. As asserted by Komaki et al. (2017), chronic diseases such as cardiac disorder, malignancy and renal impairment are seen to create inflammation in the body which leads to significant amount of loss of muscle tissues. This contributes to the expression of symptoms of malnutrition among adults. Moreover, it is seen that many diseases among the individuals prompt them to involve in restrictive diets which do not offer adequate nutrition to the body resulting in malnutrition of the individual. As argued by Cohen et al. (2016), dysphagia is the condition in which an individual requires to put in extra effort to move the food from the mouth to the stomach. The condition is associated with painful experience due to which the adults refrain to take in adequate food resulting in their malnutrition.
2.3 Concept of Stroke and Post-stroke patients
The individual experiences stroke when they have a blocked artery (ischemic) or a leak or burst in the blood vessel (hemorrhagic) which follows temporary disruption of blood to the body parts. These are often fatal in nature and can lead to permanent damage to the brain (Vahidy et al. 2016). The post-stroke condition is the recovery of the individual after the stroke. During this phase, the post-stroke patients may feel weakness, stiffness or numbness in muscles (Boussi-Gross et al. 2015). Moreover, the individuals may face emotional changes due to physical effect on the brain. The remembering, recognising and thinking ability can also be affected in the post-stroke patients. The post-stroke patients may also face issues with communication, anxiety, depression, dysphagia, visual problems, fatigue and others (Ratmansky et al. 2016).
2.4 Health issues of post-stroke patients
The post-stroke patients often face different problems with digestive tract as a result of which they face issues with eating which leads to malnutrition among them. This is because the hindrance makes the post-stroke patients feel pain to eat as they have to put force on swallowing foods and fluids (Pisegna et al. 2016). The dysphagia is also common among post-stroke patients that lead them to face difficulty in swallowing; chewing and tasting of food making them develop resentment and loss of appetite to intake proper amount of require nutrient-content food. This results them face malnutrition which deteriorates their health and leading them to experience fatal conditions.
2.5 Impact of Malnutrition on post-stroke patients
The malnutrition in post-stroke patients is to be resolved with effective approach and care from the nurses otherwise it is going to create adverse outcomes for the patient. As mentioned by J Prosser-Loose et al. (2010), energy and protein malnutrition in post-stroke patients impairs their recovery of injury in brain and other areas. This is because lack of nutrition reduces the plasticity-associated with genes which are involved in making recovery of the brain tissues after stroke. Moreover, the malnutrition is able to create abnormalities in the plasticity, functioning and structure of the fibres in the hippocampal area resulting in deteriorated health condition. The studies also revealed that malnutrition in post-stroke patients results to intensify expression of GAP-43 and trkB protein which is responsible for indicating hyperexcitability and stress response in hippocampus cavity in the brain. Further, it is found that malnutrition results post-stroke individuals to face increased amount of cerebral infarctions, decline in functional ability and increased mortality rates (J Prosser-Loose et al. 2011).
2.6 Role of nurses in preventing malnutrition in post-stroke patients
The nurses are required to play an active role in managing malnutrition among post-stroke patients so that effective interventions can be taken to resolve the issues. The issue of malnutrition is to be resolved to ensure early and better recovery of the post-stroke patients. As mentioned by Hede et al. (2016), the initial role of the nurses in preventing malnutrition among the post-stroke patients is to create nutritional screening. The nutritional screening is important as it is going to help the nurses to identify which post-stroke patients are at the risk of malnourishment or is already malnourished so that immediate interventions can be taken for them to resolve the issue. The nutritional screening is required to be arranged for 24 hours and it is to be taken as a part of general examination criteria for the post-stroke patients regarding the evaluation of their health by the nurses. The nurses required to have effective knowledge regarding the symptoms which leads to malnutrition among post-stroke individuals to prevent it. According to Academy of Nutrition and Dietetics Malnutrition, weight loss, muscles mass loss, inadequate energy intake, subcutaneous fat loss, reduced hand-grip strength and fluid accumulation are to vital factors to be monitored for detecting malnutrition (Nishioka et al. 2016). This is because early detection of the symptoms leads to immediate uptake of measure to prevent the issue of malnutrition without making it much worse for the patients to affect their health. The nurses require framing an effective nutritional plan by coordinating with doctors, dieticians and others. They require setting effective nutritional intervention and goals for the post-stroke patients by keeping in mind the adversities that may be faced otherwise by them if the nutritional goals are not fulfilled (Brown et al. 2013). This is going to help the nurses prevent malnutrition among post-stroke patients as effective monitoring and nutritional therapy may be administered to the patient by focusing on the nutritional goal. The nurses require identifying the reason for malnutrition among the post-stroke patients such as dysphagia and others (Brown et al. 2013). This is because the nurses by identifying the reason can be able to implement effective action in resolving the reasons to prevent malnutrition of the post-stroke patients helping them to lead a better and improved health. In a study by Corrigan et al. (2011), it is informed that clustered nursing is effective for post-stroke patients in resolving dysphagia. This is evident because the study shows that the experimental group who are provided clustered nursing in comparison to the control group who are delivered routine nursing showed less incidence of malnutrition and other issues as a result of dysphagia in post-stroke patients. In clustered nursing a department director, head nurse, therapists and a primary nurse is present. The primary nurse plays the role to execute primary assessment of swallowing function of the patient. The results are reported by the nurse to the doctor who according to the information suggests the nurse regarding the way to feed the post-stroke patients so that dysphagia do not pose an issue in creating malnutrition among the individuals.
Chapter 3: Research Methodology
3.0 Introduction
The methodology is framed in order to identify effective methods for conducting the study in a successful way. In order to accomplish this, information is collected from various concepts and theories explained in the previous chapter. The effective selection of research methodology is vital as it is going to show the way in which the problems identified in the study are to be resolved so that the desired objectives are obtained based on the derived results. The study is to be executed by reviewing the existing literature present to inform about the way nurses are to play their role in preventing malnutrition among the post-stroke patients. The literature review is important because it helps the researcher to develop effective knowledge regarding their area of interest which helps them to develop better focus regarding the study topic. Moreover, the review of the literature informs in a clear way about the present existing perception regarding the study topic by critically examining various information present in wider number of journal articles (Moore et al. 2015). The reviewed literature also helps the nurses to develop better information for their professional development through evidence-based practice. The evidence-based practice (EBP) is a form of problem-solving approach used for clinical decision-making regarding healthcare for the patients. It helps to integrate best available scientifically proved evidence with the best available patients and practitioner evidence in effective treatment of the patients (Greenhalgh et al. 2014). The EBP is seen to consider external and internal influences on care services and encourages thinking in a critical way for effective application of the evidence to properly care for the patients or individuals (DiCenso et al. 2014). This helps the nurses to deliver standard quality care to the patients as the review informs them to understand in which their actions can positively affect the patient.
3.1 Literature Search
The first step for executing a literature review is by completing the search of various reviewed journal, studies and other literary works related to the topic of discussion. As mentioned by Melnyk et al. (2014), using systematic approach to identify the literature works or journal articles helps to ensure that the search strategy is not compromised and executed in an organised and comprehensive way. Thus, this section is going to inform about the steps taken by the researcher to conduct the methodical searching of relevant databases, tools for identification of key terms and proper selection of journal articles to frame the current literature review.
3.1.1 Identification of keywords
In order to execute searches in a focused way, the PICO tool is to be used. According to Scells et al. (2017), PICO framework is used to identify and narrow down the key search terms to prevent the researcher from diverting away from the subject of focus. This framework also helps to identify the main concepts related to the research questions and assist to determine the exclusion and inclusion for effective development of the study. PICO stands for population, intervention, comparison and outcome.
PICO Tool

The revised PICO framework related to the study.

3.1.2 Database searches
The searching of the academic journals and updated online databases are favourable as they provide current information about the research subject in comparison to books which becomes outdated as well as become less relevant to the topic with time. As mentioned by Weinstein et al. (2017), a range of electronic databases are to be searched for identifying journal articles required for the study. This is because a single database cannot have all the quality journals or research papers required for executing the study. There are various databases that can be accessed for identifying good academic sources for researcher that includes PubMed, British Nursing Index, Google Scholar, Proquest and others. In this study, PubMed, British Nursing Index and Google Scholar are used as online database to select the primary research articles for the study. The first database used is British Nursing Index as it is the leading database in the UK that covers key nursing and midwifery journals. Moreover, the journals mentioned here are referred in English and thus no issues are faced with understanding what the journals wish to inform (proquest.libguides.com, 2018). The second database used is PubMed where large numbers of journal related to medical and nursing information are present. The website is seemed to claim that 25 millions of biomedical literature are present and it also holds the databases of Medline that us one of the leading National Library for Medicine in the US (www.ncbi.nlm.nih.gov, 2018). The third database used is Google Scholar that contains various freely accessible journal articles related to various medical studies from different publishers all over the world (scholar.google.co.uk, 2018). The databases though provided access to many relevant journals articles but many citations for further exploration were not available which were extensively related to the topic as subscriptions are required to access them. This resulted in some extent to reduce the enriched execution of the study as other relevant information which would have created better focus regarding the topic could not be accessed as they were not free.
3.1.3 Search Strategy
The searching of the articles was done initially by using keywords identified through the PICO framework. Apart from this, the search strategy used different tools such as wild characters "*" and others which acted as truncated keywords. The implementation of the symbols leads to expand the researcher includes nurses, nursing and nurse. Moreover, Boolean operators such as AND and OR are used so that the searches can b expanded or restricted.
3.1.4 Choice of research articles
Peer-review is a way by which the existing journals are reviewed to develop information above current ways of delivering care to ensure continuous professional development among nurses. As mentioned by Bertocchi et al. (2015), peer-review is way of subjecting an individual’s research ideas or information for scrutinising work of others who are in the same field before a work is published. In this study, peer review is to be used for framing the extended literature review. In order to execute this, the researcher requires having an imperative ability to evaluate practice. The peer-reviewed primary research articles are chosen because it allows the researcher to theoretically resolve any personal biases and previous ideas related to the topic that is not properly proved. As mentioned by Orleans and Manchikanti (2015), peer-reviewed articles allow avoiding inclusion of various poor and substandard research articles. In most cases, it is seen that primary research articles are peer-reviewed. In this study, the journal articles which contains primary data may it be qualitative or qualitative in nature are selected because they offer high degree of accuracy in collecting information regarding the topic. Moreover, the primary research articles are highly reliable as they are collected by reliable people in a concerned manner (McCusker and Gunaydin, 2015). The primary research articles help to offer a realistic view regarding the study topic.
3.2 Inclusion and Exclusion criteria
The application of inclusion and exclusion criteria is seen to allow executing a more concentrated search strategy related to the topic which helps to identify target studies which are able to effectively answer the raised research question. As commented by Demaerschalk et al. (2016), inclusion criteria refer to the prospective subjects related to the research and the exclusion criteria include the non-prospective objectives. The compilation of the inclusion and exclusion criteria is executed by the researcher by using PICO framework within the research questions.
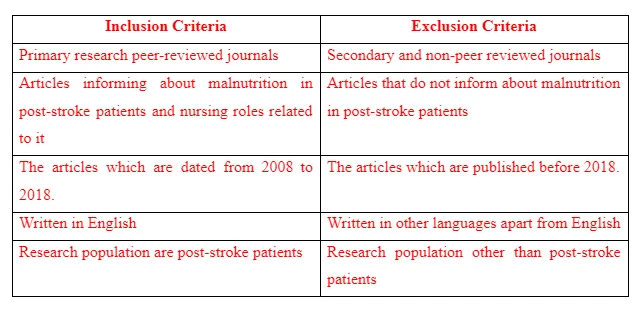
3.2.1 Justification of inclusion and exclusion criteria
The peer-reviewed articles are chosen because they follow strict publishing criteria which ensure that the information given there is authenticated in nature. Moreover, the researcher has understanding and knowledge regarding English and is not bilingual and thus articles written in English are chosen so that the researcher can understand and derive information from the articles to frame the study without error. The articles that are written within 10 years time frame are chosen because the time frame is effective enough to provide relevant and current data regarding the research topic. The literature which is found backdated more than 10 years is termed to be irrelevant due to lack of updated information (Sofi et al. 2014). Moreover, the topic focused only on malnutrition among post-stroke patients and thus other hindrances faced by the post-stroke patients were excluded as they were not relevant to the topic. The focus was no identifying the role of the nurses in preventing malnutrition thus articles which mentioned involvement of family and friends in caregiving to the posts-stroke patients to resolve malnutrition was excluded.
3.3 Data Analysis
The data analysis is required to be done in a strategic way by following logical criteria so that proper analysis is made. Thus, to fulfil this purpose the data analysis framework developed by Caldwell, Henshaw and Taylor (2011) is used. This framework for data analysis is used as it helps to provide in-depth information by analysing each aspect of the literature through proper interrogation. In this study, 15 articles are chosen out of which two articles are qualitative primary research and other 13 articles involve quantitative primary research information.
3.4 Article selection
At the initial stage, a total of 34 articles are identified out of which by using PRISMA tool it was reduced to 15 articles that were finally chosen for executing the study. The articles chosen are as follows:
Prevalence of malnutrition and its risk factors in stroke patients residing in an infirmary. Weight loss after stroke: a population-based study from the Lund Stroke Register. Contribution of ischemic stroke to hip fracture risk and the influence of gender difference. Duloxetine versus citalopram and sertraline in the treatment of poststroke depression, anxiety, and fatigue. Dysphagia, nutrition, and hydration in ischemic stroke patients at admission and discharge from acute care. Nurses’ Knowledge and Practices about Administration of Medications via Nasogastric Tube among Critically Ill Patients. Poor nutrition and alcohol consumption are related to high serum homocysteine level at post-stroke. Risk of malnutrition is an independent predictor of mortality, length of hospital stay, and hospitalization costs in stroke patients. Prevalence of dysphagia, malnutrition and dehydration at admission in a Stroke Unit, Knowledge of nurses regarding dysphagia in patients post stroke in Namibia. curationis, Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. . Clinical nursing leaders' perceptions of nutrition quality indicators in S wedish stroke wards: a national survey. Changes in nutritional state and dysphagia in stroke patients monitored during a 14-d period in a Burkina Faso hospital setting. Malnutrition and risk of malnutrition in patients with stroke: prevalence during hospital stay. (Refer to Appendix 3)
3.5 Ethical Consideration
The research is conducted by following the ethical consideration and in order to do so the guidelines mentioned in the Data Protection Act 1998 are followed. The Data Protection Act 1998 informs that no data is to be used without prior intimation to the owner or reference to them (www.legislation.gov.uk, 1998). Thus, the study has been executed by properly mentioning and referencing the names of the authors from whom information has been derived to execute the study. This helped to ensure transparency is followed in the study. In order to ensure ethical principles are followed, research integrity is ensured which means that imparity, truthfulness and fairness are maintained while analysing, collecting and interpretation of the data.
Chapter 4: Data Analysis
4.1 Thematic Analysis/ Extended Literature Review
Theme 1: Prevalence of malnutrition among post-stroke patients
The prevalence of malnutrition is one of the health issues being faced by post-stroke patients because often they experience hindrance in swallowing food and other complications. The study of Gomes et al. (2016) informs that they have taken total of 537 participants who have a mean age of 74.7 years and out of them 51% were men suffering from stroke. Moreover, among them 87% has suffered an ischemic stroke, 22% have a previous history of stroke and 34% has been diagnosed with inefficiency to effectively swallow food after stroke. On further examination, it was found that out of the total participants, 342 (64%) were at lower risk of experiencing malnutrition, 39 (7%) were at medium risk for malnutrition and 156 (29%) were at higher risk of experiencing malnutrition. This informs that all the post-stroke patients involved in the study are likely to suffer from risk of malnutrition as a potential health issue. The study also informed that post-stroke patients who are at medium risk of malnutrition are 62% likely to be readmitted, those with higher risk of malnutrition are 68% likely to be readmitted and those with low risk of malnutrition are 59% likely to be readmitted to the hospital (Gomes et al. 2016). This informs that the patients who are at medium and high risk of malnutrition post-stroke are going to show more deterioration in health as a result of which they are required to be readmitted to the hospital. The study has further informed that malnutrition in post-stroke patients are likely to be suffered by the individuals who are older, live in home without support, experience gastrointestinal diseases, face issues with mobility and others (Gomes et al. 2016). This is because older individuals often due to age-related issues apart from stroke face depression and lose taste resulting them to avoid taking adequate food (Wylie and Nebauer, 2011). Moreover, post-stroke individuals without support living in home face malnutrition because they have lower physical efficiency and lack of knowledge regarding the amount of food to be taken for their proper nutrition. In the study of Choi et al. (2015), out of 203 post-stroke patients, 84% were found to be malnourished or at the risk of malnutrition. In another study by Yoo et al. (2008), it is informed that malnutrition was experienced in 26 individuals post-stroke within 1 week who are admitted to the hospital. Moreover, the study informed that within one week improved nutrition was experienced in 4 individuals and worsened nutrition was faced by 14 individuals and no nutritional changed was seen in others. In the study of Mosselman et al. (2013), it is informed that 5% of the post-stroke patients were already malnourished, 14% of them were at risk of malnutrition and 81% were effectively nourished. However, after ten days of hospital stay, it was seen that 26% of the patients were malnourished, 39% were at risk of malnutrition and 35% were nourished. This informs that post-stroke patient face malnutrition if they are not provided proper care at the hospital as was seen in the study. It is so as the malnutrition or the risk of malnutrition increased from 9% to 65% due to ineffective care of the post-stroke patients.
Theme 2: Impact of malnutrition among post-stroke patients
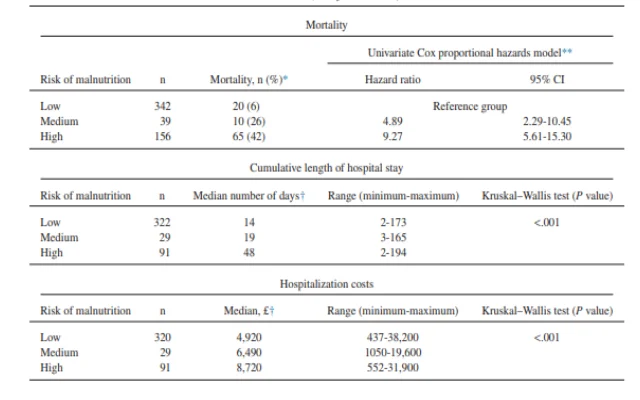
There are various advertises being faced by post-stroke patients as a result of malnutrition which deteriorates their health. In the study of Chai et al. (2008), it is informed that the post-stroke patients with malnutrition are more likely to face intense reaction of stress, show increased rate of pressure ulcers along with urinary tract infection and increased days of hospital stay. The study also informed that among 2,194 post-stroke patients who followed up for Food or Dietary Trial those were malnourished faced situation like pneumonia, gastrointestinal bleeding and other form of infections. The infection arises among them because effective nutrients required to support the better functioning of the immune system in the patients are not achieved from the diet. Thus, the immune system in the post-stroke patients fails to help them in acting against infections. In this study by Jonsson et al. (2008), it is reported that out of 305 patients reviewed in post-stroke condition it was found that 24% of the patients showed weight loss at an average of 6.6kg after 4 months and 8.3 kg on an average by 26% patients after 1 year. The study informed that the result of weight among the post-stroke patients was mainly as a result of malnutrition due to disturbed eating habits among patients. Thus, this informs that malnutrition among post-stroke patients leads them to face weight loss issues which create further complication to their health. In the study of Gomes et al. (2016), it is informed that as a result of risk of malnutrition or nutrient deficiency in post-stroke patients the length of hospital stay, mortality rates and hospitalisation costs also increases. This is evident from the study as it informs that people (322) who have low risk of malnutrition experienced 14 days increased hospital stay, in individuals with (29) medium risk of malnutrition it increased to 19 days and in individuals with high risk of malnutrition the hospitalisation stay increased to 48 days more than the normal estimate. This is because malnutrition makes the post-stroke patients to take longer time to recover from deteriorated health as a result of which the hospitalisation stay increases. This, in turn, increases the total hospitalisation cost of the post-stroke patients that may make them face financial constraints. Moreover, 20% increased mortality rate is faced by low-risk malnutrition, 10% increased mortality rate by medium risk malnutrition and 65% increased mortality rate by high-risk malnutrition post-stroke individuals. This is because malnourished post-stroke individuals lose the efficiency to cope with the deteriorated health situation caused by stroke which leads to their fatal condition.
Theme 3: Risk factors for malnutrition among post-stroke patients
In post-stroke patients, wide numbers of risk factors are present in post-stroke patients. In the study by Gomes et al. (2016), it is informed that posts-stroke patients are likely to face malnutrition because of the presence of risk factors such as elderly, has poor family condition, women, presence of malignancy, delayed rehabilitation and depression along with cognitive impairments. This is because elderly individuals are found to have reduced level of consciousness regarding which foods are to be eaten to maintain proper nutrition after stroke. Moreover, women often face reduced mobility as issues in post-stroke conditions due to which they cannot arrange proper food elements that can provide them effective nutrition, as a result, they face malnutrition. In the study of Karaiskos et al. (2012), it is informed that post-stroke patients suffer depression and takes antidepressants such as citalopram, sertraline which acts in creating a burning or dry sensation in the mouth. This is seen to make the patients face swallowing difficulty. Thus, it may be concluded that it may make post-stroke patients to face malnutrition as due to burning sensation they may refrain away from taking in adequate amount of food. The study by Crary et al. (2013) also informed that dysphagia in post-stroke patients is a potential risk for raising malnutrition among them. It is evident because it reports that dysphagia is found in 37% of patients who experienced acute stroke leading to developing malnutrition. This is because the individuals experiencing dysphagia faces hindrances in swallowing food as a result of which they refrain from taking in effective amount of food required by the body to function properly culminating in malnutrition among the patients. Moreover, it informs that posts-stroke patients may experience fatigue while eating leading them to avoid food. The post-stroke patients are also found to have reduced mobility, consciousness and weakness in the arm and legs which make them physically inefficient to take effective amount of food leading to malnutrition.

In a certain study by NHS, UK, it is found that 28-65% post-stroke individuals are likely to experience dysphagia that is linked to cause malnutrition among the patients. This is because dysphagia makes the individuals face difficulty to swallow food, as a result, the posts-stroke patients reduces food intake to avoid the hindrance and pain in forcefully swallowing the food in such condition (www.londonscn.nhs.uk, 2016). In another study of Mozzanica et al. (2018), it is informed that out of the total participants 24.2% of the posts-stroke patients are experiencing dysphagia and 16.2% of the patients are experiencing malnutrition. On further analysis, it is informed that 8 out of 39 post-stroke patients with dysphagia and 18 out of 122 patients without dysphagia are experiencing malnutrition. This informs that dysphagia is thought a potential risk factor for creating malnutrition among post-stroke patient but there are other added risk factors which are more responsible for creating malnutrition among the patients. In another study by Gomes et al. (2016), it is informed that older post-stroke patients are more likely to experience malnutrition. Moreover, the individuals who do not have any support at home in post-stroke condition and have inadequate efficiency to swallow also experience malnutrition. The study informed that 8% of the individuals with low risk for malnutrition, 5% of individuals with medium risk of malnutrition and 14% of high risk of malnutrition faced the situation due to gastrointestinal diseases in post-stroke conditions. This is because the gastrointestinal diseases led the post-stroke patients face hindrance with digestion of food and thus the post-stroke patients orients to take in less food leading to their state of malnutrition. Nearly, 19% of individuals with low risk of malnutrition, 26% with medium risk and 61% with high risk of malnutrition reports the lack of effective nutrient in their body is due to the issues of inadequacy to swallow food smoothly. Further, 8% with low and medium risk for malnutrition and 19% with high risk of malnutrition reported impaired mobility is one of the key risk faced by them to develop malnutrition. This is because restricted mobility leads the post-stroke individuals to face hindrance in taking in adequate food to resolve malnutrition. These risk factors are required to be effectively controlled so malnutrition in post-stroke individuals can be prevented.
Theme 4: Role of Nurses for preventing malnutrition among post-stroke patients
The nurses play a vital role in preventing malnutrition among the post-stroke patients because they are entrusted by the physicians to take care of the patients so that patients are able to recover from their deteriorated health condition. In order to prevent malnutrition, the initial role of the nurses is required to be focusing on the way proper amount of nutrient-rich food is to be fed to the post-stroke patients. In the study of Bath et al. (2008), it is mentioned that effective intervention is to be taken for post-stroke patients to identify how they are to be feed during their admission at the hospital. The nurses require playing the role in consultation with the doctors to identify the way of feeding so that they can act accordingly to feed the post-stroke patients to help them take nutrients in right proportion so as to prevent malnutrition. The study informs that enteral feeding is to be taken for the post-stroke patients for feeding them if they face difficulty with swallowing but the gut is effectively functional and no other complication are experienced. Thus, the nurses required to consider the fact and develop information regarding the technique to be applied to ensure proper way of enteral feeding to the post-stroke individuals who are facing issues of malnutrition as a result of dysphagia. The study also informs that weight status along with body composition in post-stroke patients is to be regularly evaluated by the nurses (Diendéré et al. 2018). This is because it is going to help the nurses in keeping a check on physical efficiency of the post-stroke individual to avoid the person from facing malnutrition by keeping a check on weight and body features that indicates malnutrition. The study has also informed that adequate protein intake is a vital aspect for the post-stroke patients to prevent them from malnutrition (Bath et al. 2008). Thus, the role of the nurses is to ensure that while feeding and providing diet to the post-stroke patients the food includes protein as one of the key nutrients besides others. In order to fulfil this purpose, the nurses require collaborating with dieticians to ensure that food given to the post-stroke patients have adequate nutrients in effective amount to prevent malnutrition among the patients. In the study of Bath et al. (2008), it is informed that post-stroke patients with extensive dysphagia are to feed through enteral nutrition with the help of a nasogastric tube or percutaneous endoscopic jejunum. The use of a nasogastric tube is also suggested for the post-stroke patients who have gastrointestinal tract obstruction or pancreatic disease. Thus, the nurses require using the nasogastric tube to feed proper nutrient supplements to the post-stroke patients so that they can be prevented from malnutrition. The study Diendéré et al. (2018) also informs the nurses are to play the role in determining the safe eating guide for the post-stroke patients so that they do not face hindrance with food. In order to fulfil this purpose, the nurses are to play the role of understanding which kind and nature of food in which way are to be delivered to the patients to prevent them from malnutrition. This is because if solid food is given to the post-stroke patients instead of liquid diet when they are facing swallowing issues the nurses are never going to be able to prevent malnutrition in post-stroke patients. It is so as they are not going to take in required amount of food due to feeling of pain from swallowing. The primary nurses are asked to monitor the post-stroke patients thoroughly from initiating eating along with the way food bolus is formed in the mouth, volume of the mouth taken in and others (Bath et al. 2008). This is because the monitoring is going to help the nurses in identifying which aspect in eating are making post-stroke patients face hindrance in eating so that they can be resolved to allow them to have effective amount of food preventing to face malnutrition. In another study by Rhoda (2015), it is informed that the nurses require delivering training to the post-stroke patients regarding the way they can effectively swallow food orally without much hindrance in a proper way. This is required to assist the post-stroke patients in the way they can have food in a proper way so that the required nutrient by the body are properly administered and they are prevented from malnutrition. The NICE guidelines mention the nurses to screen all the post-stroke patients for malnutrition at the time of admission to the hospital and after one week of hospital stay. This is required so that the post-stroke patients who are going to experience malnutrition are identified at the early stage and effective interventions are implemented to avoid the situation. The guidelines also mention the nurses to offer food, medication and fluids to the post-stroke individuals experiencing dysphagia in the form that can be swallowed by them without the hindrance of aspiration. The posts-stroke patients who are unable to take food orally within 24 hours are to be offered food through nasogastric tube by the nurses to prevent the patients from malnutrition (www.nice.org.uk, 2013). This is because it is going to help the patients get nutritious food without hindrance without letting them to experience malnutrition. Moreover, nurses are to consult with specialists dietary individuals and require developing knowledge regarding oral nutritional supplements for the post-stroke patients to prevent them from facing malnutrition.
Theme 5: Challenges faced by nurses in preventing malnutrition among post-stroke patients
The nurses face different kind of hindrance in executing care services to prevent malnutrition among post-stroke patients. In the study of Rhoda (2015), it is informed that 71.2% nurse reports lack of training is one of the key challenge faced by them in preventing malnutrition among the post-stroke patients. This is because without training the nurses are unable to use principle and techniques for preventing malnutrition among the patients. It is evident from the data received in the study where 72.8% of nurses reported they lack practical training and are not satisfied with the care given to the patients. This leads them to face hindrance in developing perception regarding the way different post-stroke patients with varied hindrances are to be managed so that they take in effective amount of nutrient-rich food to avoid malnutrition. The lack of training also leads the nurses to show lower contribution in preventing malnutrition among the posts-stroke patients resulting in their deteriorated health state. This is evident from the study by Rhoda (2015) where 93.2% of nurses reported that they require formal training to offer better care with satisfaction to the patients. This informs that the lack of training also makes them remain worried regarding the way they are feeding the post-stroke patients to understand whether the act is effective or not to prevent them from malnutrition. The confusion may lead the nurses to show lower focus in delivering effective care to the patients in turn negatively affecting their health. In the study of Abdullah et al. (2014), it is informed that nurses face hindrance in making collaboration with the multi-disciplinary team to deliver care to post-stroke patients to prevent them from malnutrition. This is because they do not know about the way services are to be shared and information is to be collected in effectively taking care of the post-stroke patients to help them recover from malnutrition or preventing them from the situation. Further, the nurses face challenges in monitoring the vital signs due to lack of training. Thus, they face hindrance in understanding whether or not the post-stroke patients are having proper amount of nutrition. Moreover, the study by Abdullah et al. (2014), also informed that nurses face hindrances in placing gastrostomy tube in feeding the post-stroke patients experiencing dysphagia which results them to face malnutrition. This is because the nurses are unable to place the tube in a proper way so that the food is transferred to the patient’s digestive tract properly. The lack of training also results the nurses in some cases to place the tube in such a way that it hurts the digestive tract of the post-stroke patients creating further deteriorating in swallowing food making it problematic for nurses to identify way to prevent malnutrition among the patients.
4.2 Strength and Limitations of Extended Literature Review
The limitation of the study by Rhoda (2015) is that it was conducted only in certain hospital in Nambia and thus the challenges faced by nurses in preventing malnutrition among posts-stroke patients in other countries or hospital remained unexplored. Moreover, the sample size small and thus the results received cannot be generalised in the nursing profession in relation to the topic. However, the strength of the study is that it has informed one of the key roles that the nurses require to perform to prevent malnutrition among posts-stroke who are facing the situation due to dysphagia. The strength of the study by Chai et al. (2008) is that it informs about the risk factors the nurses require to resolve to prevent malnutrition among post-stroke patients but the limitation is that the way nurses are going to resolve the risk factors are not informed. The strength of the study by Jonsson et al. (2008) is that it informs that weight loss is a key indicator of malnutrition among the post-stroke patients. The limitation is that the way nurses require to play their role in identifying the symptom and resolve it to prevent malnutrition is not mentioned. The strength of the study by Karaiskos et al. (2012) is that it informs what side-effects of the medication can make post-stroke patients face issues with swallowing which may lead to malnutrition among the due to intake of less amount of food. However, the limitation is that substitute medication to avoid the side-effects is not recommended for the nurses which they can give to prevent the issue. The strength of the study Crary et al. (2013) is that it informed about the aspects which creates malnutrition among post-stroke patients but the limitation is that effective evidence to help the nurses resolve the issue is not mentioned. The strength of the study by Choi et al. (2015) is that it informed the nurses to require maintaining good nutrition status so that Hyperhomocysteinemia which is related to malnutrition among post-stroke patients can be resolved. However, the limitation of the study is that they could not keep a health track of all the participants during the course of the study which may have resulted in biased or error data collection. The limitation of Gomes et al. (2016) is that it does not inform in details the length of the nutritional intervention required for the post-stroke patients to be given by the nurse to effectively prevent malnutrition. However, the strength is that the participants were not limited by age and thus a way to resolve malnutrition among post-stroke patients of any age is informed. The strength of the study Mozzanica et al. (2018) is that it has informed dysphagia is a key risk factor to malnutrition among posts-stroke patients but the limitation is that they could not produced effective evidence to prove the fact. The strength of the study by Abdullah et al. (2014) is that it informs regarding the way nurses can effectively execute their role in preventing malnutrition among post-stroke patients by resolving the challenges they are facing. However, the limitation is that evidence of success for the implementation of the strategies to resolve the challenges are not present. The strength of the study by Bath et al. (2008) is that it informs regarding the way nurses can use feeding tubes to ensure proper amount of food is given to post-stroke patients with swallowing difficulties to prevent malnutrition. However, the limitation is that the study do not inform diet chart to be followed by the nurses to ensure better nutrition among the patients. The limitation of the paper by Yoo et al. (2008) is that that the study is executed in a single hospital at a particular country and thus the diet chart to be followed by the nurses in other countries to prevent malnutrition among post-stroke patients is not mentioned. The strength is that nurses know that following proper dietary supplements malnutrition in posts-troke patients can be prevented. The strength of the study by Persenius et al. (2015) is that it informs the implication of roles by nurses to be executed to prevent malnutrition among post-stroke patients. However, the limitation is that the study information cannot be generalised for nurses in other countries apart from Sweden as it is only a nationwide survey. The strength of the paper by Diendéré et al. (2018) is that it informs about the prevalence of malnutrition among post-stroke patients and reasons for the situation for the nurses to perceive the situation to be of vital importance. However, limitation is that role of nurses to resolve the situation is not explained. The limitation of the study by Mosselman et al. (2013) is that it do not inform about the way screening is to be made by the nurses to prevent malnutrition among post-stroke by taking early intervention. However, the study strength is that it mentioned that nurses require screening post-stroke to identify factors that are causing malnutrition among them.

Chapter 5: Conclusion and Recommendation
5.1 Conclusion
The above discussion informs that malnutrition is the condition that creates deficient presence of essential nutrients in the body required for effective functioning. The post-stroke patients are those who have already suffered stroke and are trying to recover from the situation to have better health. However, it is reported that malnutrition is faced by most of the post-stroke patients as they face issues with swallowing food properly. The lack of effective support, dysphagia, depression and stress from deteriorated health situation and other factors are contributing to their malnourished state. The study informs that the issue of malnutrition among the post-stroke patients can be effectively resolved with intervention by the nurses. The nurses are required to play the role of implementing different feeding techniques for specific post-stroke patients according to their health issue and efficiency of eating food to deliver proper amount of nutrients to the body. Moreover, the study informs nurses to play their role of screening and monitoring the nutrient status of the post-stroke patients to ensure that none face malnutrition. The nurses are also required to play the role of identifying which texture and nature of food are to be provided to which post-stroke patients by consulting with the doctors, dieticians and others to prevent malnutrition among the patients.
5.2 Recommendations
Training:
The nurses involved with managing posts-stroke patients are recommended to be effectively trained to have adequate knowledge regarding identification of signs and symptoms related to swallowing difficulties in posts-stroke patients which are leading the patients to malnutrition. This is because it is often found that lack of knowledge about identifying the difficulties the nurses force the patients to eat food in the normal way which results them to avoid intake of sufficient food to get nutrient resulting in malnutrition. It is also recommended that nurses receive a formal and compulsory training regarding the foods to be avoided and given to the posts-stroke patients to improve their health.
Monitoring of nutritional status:
The nurses are recommended to execute regular monitoring of the nutritional status of the post-stroke patients. This is required so that the post-stroke patients who are undernourished can be effectively identified in the early stage so that they can be prevented from malnutrition. For this purpose, the nurses are recommended to following the parameters such as biochemical measures of glucose and pre-albumin, swallowing status, eating dependence and assessment, unintentional weight loss and extent of nutritional intake. These parameters are to be regularly monitored so that the best feeding technique can be applied for the post-stroke patients by the nurses to help them avoid malnutrition. Moreover, the nurses are recommended to ensure that the food texture given to the posts-stroke patients with swallowing difficulty are properly maintained so that they do not face difficulty in eating.
Knowledge regarding Feeding Techniques and hygiene:
The nurses are recommended to have effective knowledge regarding the way to feed different post-stroke patients according to their swallowing ability to prevent them from malnutrition. This is because all posts-stroke patients may not swallow food properly. In this cases, the nurses are required having knowledge regarding the way to manage the nasogastric tube to feed the patients. This is because without proper knowledge the nasogastric tube may not be properly placed that may lead to aspiration issues with the patients. Moreover, the nurses are recommended to manage proper hygiene and clean the nasogastric tube accordingly along with requires checking no blockage is present in the tuber before feeding the patient. The nurses are also recommended to make non-verbal contact with the patients such as maintaining good eye contact, leaning forward while feeding them and other non-verbal gestures. This is required to make the post-stroke patient feel ease while eating.
Collaborative working:
The nurses require working collaboratively with the multi-disciplinary team to offer effective care to the post-stroke patients so that they are prevented from malnutrition. This is because nurses with consultation with the doctors and speech pathologist would be able to assist the post-stroke patients to overcome swallowing difficulty which may be avoiding them from taking proper amount of food leading them to malnutrition. The nurses while working in collaboration with the multi-disciplinary team would be able to develop knowledge regarding what kind of diet and which foods are to be given to each of the posts-stroke patients according to their medical condition. This would help the nurses to maintain a nutrient-rich diet for the post-stroke patients thus assisting them to prevent rise of malnutrition among the patients.
References
- Abdullah, M., Mohammed, W. and Ismail, M., 2014. Nurses’ Knowledge and Practices about Administration of Medications via Nasogastric Tube among Critically Ill Patients. Journal of Education and Practice, 5(1), pp.147-159.
- Arsava, E.M., Aydoğdu, İ., Güngör, L., Işıkay, C.T. and Yaka, E., 2018. Nutritional Approach and Treatment in Patients with Stroke, An Expert Opinion for Turkey. Dysphagia, 25(26), p.30.
- Boussi-Gross, R., Golan, H., Volkov, O., Bechor, Y., Hoofien, D., Schnaider Beeri, M., Ben-Jacob, E. and Efrati, S., 2015. Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy. Neuropsychology, 29(4), p.610.
- Chai, J., Chu, F.C.S., Chow, T.W. and Shum, N.C., 2008. Prevalence of malnutrition and its risk factors in stroke patients residing in an infirmary. Singapore medical journal, 49(4), p.290.
- Choi, S.H., Choi-Kwon, S., Kim, M.S. and Kim, J.S., 2015. Poor nutrition and alcohol consumption are related to high serum homocysteine level at post-stroke. Nutrition research and practice, 9(5), pp.503-510.
- Cohen, D.L., Roffe, C., Beavan, J., Blackett, B., Fairfield, C.A., Hamdy, S., Havard, D., McFarlane, M., McLauglin, C., Randall, M. and Robson, K., 2016. Post-stroke dysphagia: A review and design considerations for future trials. International Journal of Stroke, 11(4), pp.399-411.
- Collins, J. and Porter, J., 2015. The effect of interventions to prevent and treat malnutrition in patients admitted for rehabilitation: a systematic review with meta‐analysis. Journal of human nutrition and dietetics, 28(1), pp.1-15.
- Correia, M.I., Hegazi, R.A., Diaz‐Pizarro Graf, J.I., Gomez‐Morales, G., Fuentes Gutiérrez, C., Goldin, M.F., Navas, A., Pinzón Espitia, O.L. and Tavares, G.M., 2016. Addressing disease‐related malnutrition in healthcare: a Latin American perspective. Journal of Parenteral and Enteral Nutrition, 40(3), pp.319-325.
- Diendéré, J., Millogo, A., Preux, P.M., Jésus, P. and Desport, J.C., 2018. Changes in nutritional state and dysphagia in stroke patients monitored during a 14-d period in a Burkina Faso hospital setting. Nutrition, 48, pp.55-60.
- Gomes, F., Hookway, C. and Weekes, C.E., 2014. Royal C ollege of P hysicians I ntercollegiate S troke W orking P arty evidence‐based guidelines for the nutritional support of patients who have had a stroke. Journal of human nutrition and dietetics, 27(2), pp.107-121.
- Hede, G.W., Faxén-Irving, G., Olin, A.Ö., Ebbeskog, B. and Crisby, M., 2016. Nutritional assessment and post-procedural complications in older stroke patients after insertion of percutaneous endoscopic gastrostomy–a retrospective study. Food & nutrition research, 60(1), p.304-356.
- Malone, A. and Hamilton, C., 2013. The Academy of Nutrition and Dietetics/the American Society for Parenteral and Enteral Nutrition consensus malnutrition characteristics: application in practice. Nutrition in Clinical Practice, 28(6), pp.639-650.
- Mangus, R.S., Bush, W.J., Miller, C. and Kubal, C.A., 2017. Severe sarcopenia and increased fat stores in pediatric patients with liver, kidney, or intestine failure. Journal of pediatric gastroenterology and nutrition, 65(5), pp.579-583.
- Melnyk, B.M., Gallagher‐Ford, L., Long, L.E. and Fineout‐Overholt, E., 2014. The establishment of evidence‐based practice competencies for practising registered nurses and advanced practice nurses in real‐world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews on Evidence‐Based Nursing, 11(1), pp.5-15.
- Mosselman, M.J., Kruitwagen, C.L., Schuurmans, M.J. and Hafsteinsdóttir, T.B., 2013. Malnutrition and risk of malnutrition in patients with stroke: prevalence during hospital stay. Journal of Neuroscience Nursing, 45(4), pp.194-204.
- Nishioka, S., Wakabayashi, H., Nishioka, E., Yoshida, T., Mori, N. and Watanabe, R., 2016. Nutritional improvement correlates with recovery of activities of daily living among malnourished elderly stroke patients in the convalescent stage: a cross-sectional study. Journal of the Academy of Nutrition and Dietetics, 116(5), pp.837-843.
- Pisegna, J.M., Kaneoka, A., Pearson Jr, W.G., Kumar, S. and Langmore, S.E., 2016. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clinical Neurophysiology, 127(1), pp.956-968.
- Scells, H., Zuccon, G., Koopman, B., Deacon, A., Azzopardi, L. and Geva, S., 2017, November. Integrating the framing of clinical questions via PICO into the retrieval of medical literature for systematic reviews. In Proceedings of the 2017 ACM on Conference on Information and Knowledge Management (pp. 2291-2294). ACM.
- Steele, C.M., Bayley, M.T., Peladeau-Pigeon, M., Nagy, A., Namasivayam, A.M., Stokely, S.L. and Wolkin, T., 2016. A randomized trial comparing two tongue-pressure resistance training protocols for post-stroke dysphagia. Dysphagia, 31(3), pp.452-461.
- Vahidy, F.S., Parsha, K.N., Rahbar, M.H., Lee, M., Bui, T.T., Nguyen, C., Barreto, A.D., Bambhroliya, A.B., Sahota, P., Yang, B. and Aronowski, J., 2016. Acute splenic responses in patients with ischemic stroke and intracerebral hemorrhage. Journal of Cerebral Blood Flow & Metabolism, 36(6), pp.1012-1021.
- Wu, C.H., Liou, T.H., Hsiao, P.L., Lin, Y.C. and Chang, K.H., 2011. Contribution of ischemic stroke to hip fracture risk and the influence of gender difference. Archives of physical medicine and rehabilitation, 92(12), pp.1987-1991.
- Yoo, S.H., Kim, J.S., Kwon, S.U., Yun, S.C., Koh, J.Y. and Kang, D.W., 2008. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Archives of neurology, 65(1), pp.39-43.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



