Navigating the Seas of Knowledge
Introduction
A literature review is a search and evaluation of the existing literature in your selected topic area or subject. It establishes the current state of knowledge in the field of the issue or topic you're writing about. There are four basic goals of a literature review:
It examines the literature in your field of study.
It compiles a summary of the information found in the literature.
It critically evaluates the data acquired by identifying knowledge gaps, demonstrating the limitations of ideas and points of view, identifying opportunities for further research, and analysing areas of contention.
It arranges the literature in a logical manner.

The frequency of falls among older people ranges average between 28-35% of people aged 65 fall each year. For those more than 70 years, the fall rate has increased to a range between 32-42% (Sirohi et al, 2017). The frequency of falls increases with age, older people who reside in nursing homes get, the easier it becomes for them to fall more often than those living in their communities surrounded by relatives. The rate of fall injuries and hospital admission due to falls for people aged 60 years and above in Australia, Canada, and the United Kingdom of Great Britain and Northern Ireland ranges from 1.6 to 3.0 per 10,000 population total (Kaminska et al et al, 2018). Medical attention has shifted focus to public health problems that are associated with falls and the related injuries. The falls lead to 30% of mild to severe injuries, hip fractures, traumatic brain injuries, and upper limb injuries resulting from falls. The duration of hospital stay for these injuries varies depending on the magnitude of the fall and the damages it has caused (Reist el al., 2017). For students conducting research in the field of healthcare, exploring the implications of preventive measures is very essential. Seeking healthcare dissertation help provide them valuable insights into addressing this concern.
This paper reviews literature on the how to minimise the risk of falls among the elderly in-home settings with special emphasis on polypharmacy.
Search strategy
The topic of how to minimize falls among the elderly in-home settings is complex and requires a lot of research. Journals and articles from Medline, CINAHL, and PubMed were used to inform this research. (Aveyard & Sharp, 2017). Other databases that contained relevant data that informs the topic under study were used. PICO framework was also used to identify key terms used in the search strategy of this paper. Keywords such as "fall prevention" OR "prevention of falls" OR "fall," "elderly" OR" geriatric" OR "older person," OR "polypharmacy," OR "multiple drugs" were used to locate these search papers. To narrow down the research, search terms such as the relationship between falls and Polypharmacy were used.
Inclusion and exclusion criteria
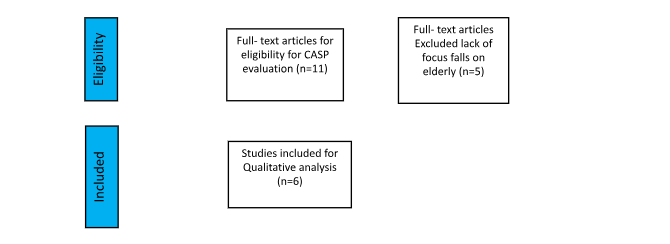
The search was only restricted to united kingdom countries and Poland. Five articles used were from the UK, while 1 article was from Poland. Data used was from electronic sources, which allowed the literature search. The omitted article was outside England and Poland, written in a language that was not English (Eriksen, Mette & Frandson, 2018). Articles that were published more than 5 years ago were omitted in the study. More than 6344 studies were screened, and only 6 of them were appropriate for review. The rest were missed due to geographical location, language barrier, date of publication, and insufficient information on the topic of study.
PRISMA flow diagram

PICO Table
This evidence-based medicine guide helps health professionals and learners enhance their efficiency and effectiveness in using medical literature.


Literature Review
Dhalwani and his colleges researched the association between Polypharmacy and falls among the elderly in England. With the varying demographics and increase in the older population in the last few decades, falls have been common in patients under home care. This has become an important public health issue. Participants for this study were recruited from households included in 1998, 1999, and 2001. These patients had follow-ups from nurses with detailed health examination reports. These visits took place every four years. To maintain the overall representation of participants between 50-53 years, refreshment samples were added at the wave of 3, 4, and 6. Those interviewed at the wave of 6 were 9,169 people (Dhalwani et al., 2017). The study population from the 6th wave took place in 2012 to2013 for people aged 60 and above. These individuals were included in the nurses’ visits as drug and polypharmacy information was collected in this wave. A follow-up data and assessment was done in wave seven from 2015 to 2016.
The respondents in wave six were asked to name all the drugs prescribed to them. Those with cognitive or physical impairments were eligible for proxy interviews. The names of the medications asked were recorded by nurses and assigned a code according to the British National Formulary (BNF). To verify the self-reported medication use, the nurses checked the containers. Six digit codes were used to reflect the three classification levels in the BNF section 10.1.1, which was coded as 100101. Blood glucose monitoring equipment, dressing and urinary devices were excluded (Dhalwani et al., 2017). Participants who had experienced falls in wave7 more than 50 times for the last two years were excluded from the study. Population characteristics such as body weight, sex, ethnicity, and health status were summarised using statistical analysis. It was concluded from the above research that a5213 participants provided data in both waves 6 and 7 on Polypharmacy and falls. Using different thresholds to define Polypharmacy, it was deduced that less than or equal to 4 drugs and adjusting to lifestyles and socio-demographic factors, the rate of falls was higher in individuals with Polypharmacy compared to those without. Using drugs was associated with 50% higher rates of falls.
A similar study to Dhalwani and his colleagues was conducted by Cheonga et al. (2018). He focused more on medical-related risk factors that were associated with repeated hospital admissions in frail elderly. Repeated hospital admissions are prevalent in older people. The major risk factor of these falls leading to hospital admissions is medication. The main objective of this study was to examine the association between medication-related risks and the repeated hospital admissions in older people living with frailty. A retrospective case study control was carried out on a total of 200 people who were aged 75 and above. These individuals had unplanned medical admissions in large hospitals in England in 2015 between January and December (Cheong et al., 2018). From the discharge summaries, data on demographic, clinical, and medical-related were obtained. Statistical comparisons were made between patients with more than three hospital admissions and those with less than 2. Those with more than three admissions were used as case studies, while those with less than two admissions were used as control experiments. To identify the independent predictors of repeated hospital admissions, regression analysis was used. The mean age of these participants was 83.8 years, of which 65 % were females. There were a total of 561 admissions across the sample selected for the study. Those admitted due to respiratory problems were 25%, while 17% were admitted due to falls (Cheong et al., 2018). The use of Univariate logistic regression suggested that five medication-related risks were associated with these repeated medical admissions. Medication-related chances may play a role in future repeated admissions due to falls. These highlights are significant opportunities to improve health outcomes as a result of medical-related risks.
Bartoszek et al. (2018) researched falls among the elderly and their connection with polypharmacy and polypragmasy. Falls had become part of the great geriatric problem in Poland at this time, which had resulted in decreased functionality capacity, which negatively impacted the quality of life. The main aim of this research was to describe the problems of falls among the elderly, with a particular emphasis on the recurring episode of falls. Advanced old age is among the risk factors that are associated with falls. Old age leads to blurred vision, hearing impairments, and changes in body shape and stability. Bartoszek depicted that falls were more recurring in people aged 65 and above living at home. More than 35% of this age experienced falls at least once a year (Bartoszek et al., 2018. Those above 80 years experienced 405 falls, while those at 90 years had a higher percentage of falls than the rest. In more than half of these cases, there are recurrent falls. In the Poland senior survey, 23.15 of the people who were 65 years and above experienced falls, most of whom were females. It has been deduced that the frequency of falls increases with age. Half of these falls occurred while at home, with most of them occurring during the day. The number has been projected to double by 2050. An older adult with Polypharmacy requires adaptation of comprehensive therapeutic regimes with the use of drugs. This study finds that a combined effect of drugs and age forms a risk factor for recurring falls, especially for those individuals at home.
Muray and his colleges in 2017 carried out a study on fall prevention strategies in emergency departments in the UK. This study aimed to determine the need for the implementation of fall prevention studies in emergency departments. The risk fall assessment tool was based on the Morse Fall Scale (MFS); a mixed-gender aged 65 and 80 years and above was used for assessment. Six risks (age, Osteoporosis, alcohol, vision impairments, altered elimination patterns, seizure history, and previous falls) assessment variables were analysed using the MFS. A logical regression analysis was used to test the predictor strength relationship between the variables (Muray et al., 2017). The findings depicted that a total of 5,371 generic outpatients were at risk of falls. Women have higher chances of fall incidences in both the young and old age categories. Being on medication for patients aged 80 and above also increased the risk of falls in both genders. According to the regression analysis performed, the six variable tools accounted for 73-98% of falls. The implementation strategy requires that hospital staff develop and adhere to fall prevention policies to support a safe patient environment and physical status. It involves extensive education and support to patients and families from nurses and pharmacists. An updated care plan regarding medical care should be available to every person. Precaution measures to patients with a vulnerable cognitive condition are essential for life.
Hammond and Wilson conducted research in (2017) on Polypharmacy and falls among the elderly. The main aim of the study was to establish the relationship between Polypharmacy and falls among the elderly. Polypharmacy has become common among the elderly although it can be therapeutic, it is linked to events that have led to falls. 65 years and above falls were 2.8 times common in individuals with blood pressure below 140 mm Hg compared to those with greater blood pressure greater than or equal to 140 mm Hg. According to research, it is proven that the probability of falls increases with the increases in the rate of antidepressants taken in by the elderly. Sedatives and anti-epileptic drugs increase the likely hood of recurrent falls by twice folds. An elder person taking cardiovascular drugs such as nitrates have more likely to experience recurrent falls (Hammond & Wilson et al., 2017). Hence it’s evident that Polypharmacy has increased the likelihood of falls among the elderly from 1.5 to 2 times. The use of sedatives, hypnotics, anticholinergic and anti-diabetics agents' among the elderly increases the risk of falls. These drugs can cause fainting, collapse, and as a consequence, slipping or falling. 30-50 % of individuals living in long-term care institutions fall each year, and averagely 40% of them experience these recurrent falls. These incidences vary among countries of origin; about 31% of the elderly in china fall each year on average. In the US, the proportion of elders who fall each year ranges from 21.6% in Barbados to 34% in Chile.
From the study conducted by Richardson in 2015, it was established that of the 1611 participants with Polypharmacy, 569 cases were reported to at least have one fall within the past 2 years. Of the 3,602 participants without Polypharmacy, 875 patients were reported to have at least fallen. A 21% increment has been reported in people with Polypharmacy compared with people without Polypharmacy. For those using drugs, it was reported that the rate of falls was 18% higher in individuals with Polypharmacy compared with those without. Patients that use 10 or more drugs are associated with a 50% higher rate of falls. Observation analysis was able to establish that 231 falls occurred per every 1000 persons that were reported. Polypharmacy, including antidepressants, was associated with a greater risk of falls, injurious falls, and a greater number of falls. Still, the antidepressants use without the condition, and Polypharmacy without antidepressants was not (Richardson, 2015). Other medications were also assessed to determine whether they had an impact on the occurrence of falls. Hence it was established that in middle-aged individuals and older adults, Polypharmacy, including antidepressants or Benzodiapine, greatly contributed to the number of falls.
Implementation strategies
In an effort to reduce falls among the elderly, optimizing health, participation, and security opportunities to enhance the quality of life is needed. It depends on a variety of determinants that surround individuals, families, and communities (Zaminitto et al, 2020). Biological factors also play a significant role in preventing individuals from falls and injuries that occur as a result. Functional capacity such as muscular strength and cardiovascular output increases the childhood peak in early adulthood hence decline. Lifestyle and environmental factors surrounding an individual greatly influence the rate of decline in adult falls (Womack et al, 2019).
Regular exercise
Exercise is an important factor that is recommended in controlling the occurrence of adult falls. Optimum levels of physical activities during childhood and adolescence are important for developing healthy bones. As individuals age, they experience a drastic decline in bone mass. This that manages to keep a healthy lifestyle can slow down the process. Women who are past the menopause stage require a healthy lifestyle to counterbalance the hormonal content that may cause Osteoporosis (Bartozek et al., 2018).
You may be at risk of falling or stumbling if you have a medical condition or are an older adult. Broken bones or even more catastrophic injuries can ensue as a result of this. Exercising can help you avoid falling because it strengthens and stretches your muscles, improves your balance, and extends the amount of time you can be active. The exercises can be done practically anywhere and at any time (Cheonga et al., 2020). As you gain strength, consider holding each position for extended periods of time or adding light weights to your ankles. This will improve the exercise's effectiveness. Aim for 150 minutes of exercise every week. Do muscle-strengthening workouts at least twice a week. Start carefully and consult your doctor to ensure you're performing the proper exercises for you. You can either exercise alone or join a group. Always remember to breathe slowly and easily when exercising. Do not take a deep breath.
Balance exercises can be performed on a daily basis. Try balancing on one foot while in line at the store. Attempt to sit and stand without using your hands. Stand on your toe exercises are also recommended. Hold on to a solid support for balance, such as the back of a chair, to strengthen your calves and ankle muscles. Stand with your back straight and your knees slightly bent. As high as you can, get on your tiptoes (Le et al, 2021). Lower your heels to the ground slowly. This can be done repeatedly (10–15 times) more. Across a wide range of baseline participant characteristics and exercise procedures, exercise is beneficial in avoiding fall-related injuries. Exercise is linked to a low injury rate and high compliance, implying that it is a viable strategy for controlling fall-related injuries.
Conclusion
The research paper focuses on the relationship between falls and the use of Polypharmacy among older adults in society. It has been established that there is a strong relationship between these two variables with age as the variable used to measure intensity. With age come other opportunistic diseases such as hypertension, cancer, ulcers, and heart diseases. These diseases are regulated by taking drugs prescribed to them by different physicians. Reaction resulting from taking multiple medications by elderly people is more diverse and intense than young people. The side effects are also adverse and may lead to slipping or falling. Falls also negatively impact older people. The fear of falling by these individuals results in a reduction in physical activities due to worry. This in turn, leads to depression and stress as the 'Fear of Fall' is instilled in them. It has been deduced that falls are directly related to Polypharmacy. Elderly people with the condition require comprehensive exercise regimes with drugs recommended to them by a different specialist it leads to Polypragmasy. Polypharmacy involves taking more than four drugs, while Polypragmasy consists in taking in one drug with no clinical indication. Drug reactions are more adverse in adults than in the young population, with the increased the chances of diseases to elderly people demand that they take in multiple drugs. These drugs may include those prescribed as well as those which are over the counter and hence the side effects. These side effects maybe in form of dizziness of drowsiness that may lead to falling.

References
Alshammari, S. A., Alhassan, A. M., Aldawsari, M. A., Bazuhair, F. O., Alotaibi, F. K., Aldakhil, A. A., & Abdulfattah, F. W. (2018). Falls among elderly and its relation with their health problems and surrounding environmental factors in Riyadh. Journal of family & community medicine, 25(1), 29.
Bartoszek, A., Sagan, A., Korga, W., & Szalast, K. (2018). Falls among elderly and their connection with Polypharmacy and polypragmasy. Journal of Education, Health and Sport, 8(8), 667-673.
Cheonga. V, Sowtera J, Scallyb, A.,Hamiltonc,N., Alid,A, Silcocka J.(2018). Medication-related risk factors and its association with repeated hospital admissions in frail elderly: A case control study https://doi.org/10.1016/j.sapharm.2019.02.001.
Dhalwani, N. N., Fahami, R., Sathanapally, H., Seidu, S., Davies, M. J., & Khunti, K. (2017). Association between Polypharmacy and falls in older adults: a longitudinal study from England. BMJ open, 7(10), e016358.
Eriksen, M. B., & Frandsen, T. F. (2018). The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. Journal of the Medical Library Association: JMLA, 106(4), 420
Ie, K., Chou, E., Boyce, R. D., & Albert, S. M. (2021). Fall risk-increasing drugs, Polypharmacy, and falls among low-income community-dwelling older adults. Innovation in aging, 5(1), igab001.
Kamińska, M. S., Miller, A., Rotter, I., Szylińska, A., & Grochans, E. (2018). The effectiveness of virtual reality training in reducing the risk of falls among elderly people. Clinical interventions in aging, 13, 2329.
Kratz, T., & Diefenbacher, A. (2019). Psychopharmacological treatment in older people: avoiding drug interactions and Polypharmacy. Deutsches Ärzteblatt International, 116(29-30), 508.
Matchar, D. B., Duncan, P. W., Lien, C. T., Ong, M. E. H., Lee, M., Gao, F., ... & Eom, K. (2017). Randomized controlled trial of screening, risk modification, and physical therapy to prevent falls among the elderly recently discharged from the emergency department to the community: the steps to avoid falls in the elderly study. Archives of physical medicine and rehabilitation, 98(6), 1086-1096.
Midão, L., Giardini, A., Menditto, E., Kardas, P., & Costa, E. (2018). Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Archives of gerontology and geriatrics, 78, 213-220.
Muray, M., &. Bélanger, C., H. (2016). Fall prevention strategy in an emergency department. Laurentian University, Sudbury, Canada, and College of Business Administration.
Reis, K. M. C. D., & Jesus, C. A. C. D. (2017). Relationship of Polypharmacy and polypathology with falls among institutionalized elderly. Texto & Contexto-Enfermagem, 26.
Richardson K., K. B. (2015). Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults. national Library of Medicine .
Sirohi, A., Kaur, R., Goswami, A. K., Mani, K., Nongkynrih, B., & Gupta, S. K. (2017). A study of falls among elderly persons in a rural area of Haryana. Indian journal of public health, 61(2), 99.
Womack, J. A., Murphy, T. E., Rentsch, C. T., Tate, J. P., Bathulapalli, H., Smith, A. C., ... & Justice, A. C. (2019). Polypharmacy, hazardous alcohol and illicit substance use and serious falls among PLWH and uninfected comparators. Journal of acquired immune deficiency syndromes (1999), 82(3), 305.
Zaninotto, P., Huang, Y. T., Di Gessa, G., Abell, J., Lassale, C., & Steptoe, A. (2020). Polypharmacy is a risk factor for hospital admission due to a fall: evidence from the English Longitudinal Study of Ageing. BMC public health, 20(1), 1-7.
Looking for further insights on Mitigating Misinterpretation, and Ensuring Authenticity? Click here.
- 24/7 Customer Support
- 100% Customer Satisfaction
- No Privacy Violation
- Quick Services
- Subject Experts



